

A surprising herpesvirus virus shows up in fibromyalgia patients’ guts
However similar the symptom presentations of fibromyalgia (FM) and chronic fatigue syndrome (ME/CFS) are, their research pathways have been fairly distinct, with FM researchers focusing more on the central nervous system and ME/CFS researchers more on pathogens, the immune system, and energy production.
Despite the fact other herpesvirus can infect the gut lining Carole Duffy found only HSV-1 in the fibromyalgia biopsies (from Thomas-Splettstoesser-Wikimedia Commons)
As time has gone on, though, the fields have started to coalesce a bit. It took years, for instance, for the small fiber findings in FM to filter down to ME/CFS, but they were recently documented in ME/CFS. Similarly, FM researchers have shown more interest in the immune system and orthostatic intolerance of late.
Pathogens, though, have remained almost entirely the province of ME/CFS research. While herpesvirus ME/CFS papers continue to pour out – one was published just last month – the number of herpesvirus FM studies, most of which date back decades, can be counted on the fingers of one hand.
All of which makes the herpes simplex virus type 1 (HSV-1) saga in fibromyalgia all the more inexplicable. For one, the herpesvirus Skip Pridgen MD has proposed is causing FM has been virtually ignored by both fields. Despite that fact, Pridgen has been able to do something for FM that no one in the ME/CFS field – despite decades of interest, and dozens and dozens of herpesvirus studies and papers – has been able to do: mount a large (n=460, 40+sites), rigorously controlled, trial of anti-herpes virus drugs. (The closest ME/CFS came to that was the single-site, 30-person Montoya valganciclovir trial in 2013). It’s an amazing thing.
Learn more about HSV-1…
A New Virus for Fibromyalgia (and ME/CFS?)
The Gist
- Skip Pridgen’s assertion that herpesviruses may be causing fibromyalgia was – given that no one in 30 years had cared a darn about herpesviruses in FM in 30 years – was bad enough. If that seemed wild then Pridgen’s belief that herpes simplex virus-1 (HSV-1) was behind FM seemed beyond the pale given that no one in the herpesvirus-focused ME/CFS research field had given that virus a thought.
- This latest study, though, led by Carole Duffy, found that not only was active HSV-1 found in ALL the gut biopsies of FM patients with gut problems but that it was the ONLY herpes virus found.
- While other herpesviruses can infect the gut lining, HSV-1 is the only herpesvirus known to infect the neurons leading to the gut. Because HSV-1 can spread across the synapses of the neurons it can potentially affect many neurons and has been found to infect the trigeminal neurons in the face, among others. Pridgen has proposed that HSV-1 infects more than the gut in FM.
- The high rates of HSV-1 (80%) found in the biopsies of people with functional gastrointestinal disorders (gut disorders produced by problems with the gut-brain axis) suggested HSV-1 might be producing problems in people with mysterious gut issues (such as IBS, nausea, vomiting and many others). One possibility is that viral interference with gut-brain interactions is altering gut motility, affecting gut flora, etc.
- In contrast, the low rates of HSV-1 found in people with gut issues but who did not have a functional gastrointestinal gut disorder suggested HSV-1 was probably not causative.
- Since the study focused on gut biopsies from FM patients with gut issues we don’t know if the results apply to FM patients without these issues. We’ll find out more about that when the results of Pridgen’s big FORTRESS antiviral trial in FM are released in September. (That trial was not restricted to FM patients with gut issues).
- Virios, the company Pridgen started, has begun a trial of a similar product (valacyclovir/celexicob) in long COVID at the Bateman Horne Center in Salt Lake City.
The study, led by University of Alabama virologist Carole Duffy, examined gastric biopsies from 30 people who met the criteria for having both a functional gastrointestinal disorder (FGID) and fibromyalgia, 15 people with an FGID but not with FM, and 15 control patients who had undergone an endoscopy for something other than a functional gut issues (GI bleed, anemia, hiatal hernia, cancer, etc.).
The Functional Gut Diseases
Functional gastrointestinal disorders (FGIDs) are generally characterized as disorders such as irritable bowel syndrome that impact functionality but for which no organic problem has been found. They’ve have been found in every part of the gastrointestinal system. The dozens of FGIDs that have been identified produce problems with belching, esophageal pain, vomiting, nausea, gallbladder issues, rectal pain, etc. Perhaps due to the complex nature of its internal nervous system – sometimes referred to as the “second brain” – the gut seems to be superb at producing mysterious forms of the disease.
Our understanding of FGID has been evolving over time, and the authors note that problems with gut motility (the timely passage of materials through the gut), damage to the gut lining, immune problems, and altered gut flora (microbiome) are now believed to contribute to them.
As to what causes them – anything that disturbs gut-brain communications or alters gut immune functioning, and/or dysregulates the neuroendocrine system could be responsible. At the top of that list are parasitic, bacterial, or viral infections. Of the viruses, the herpesviruses – most of which we never manage to completely eliminate – and which readily infect the gut and can certainly impact the neuroendocrine system, of course, loom large.
Several herpesviruses (EBV, varicella-zoster, cytomegalovirus) can infect the gut lining, but only HSV-1 has been able to make it to the neurons that innervate the gut. Once an infection there is established, any reactivation of the virus will cause the production of more virions which then attack the gut lining as well as gut-brain-neural pathways.
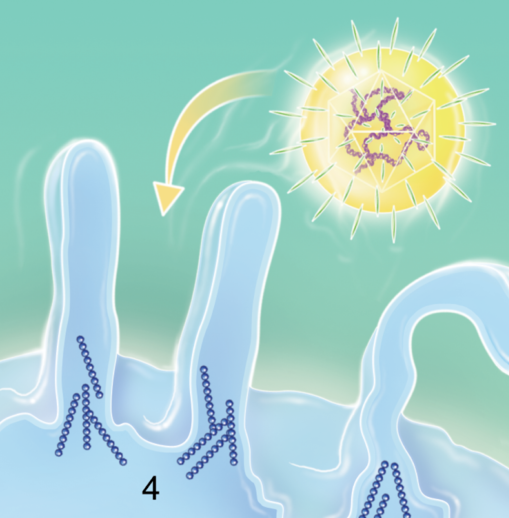
Herpes simplex virus infecting cells (from Gigo et. al. Wikimedia_commons)
When Pridgen’s standard gut treatments for his FM patients produced a relapsing-remitting pattern – they got better and then relapsed – he suspected viruses were at play. The big surprise came when their gut and FM symptoms improved while on his antiviral combination. Pridgen believes the HSV-1 infection he’s found in the gut is just the tip of the iceberg.
The virus is best known for producing cold sores but can infect sensory nerves in the trigeminal ganglia in the face, the gut, and nerves that make up the gut-brain axis. The bug apparently first enters the body through the mouth and the throat, and makes it down to the gut when we swallow.
Animal studies have shown that HSV-1 infection of the major nerve leading to the gut (myenteric plexus) results in “functional and structural alterations of the enteric (or gut) nervous system”. Interestingly, the virus didn’t need to replicate to affect the gut – all it needed to do was emit a substance that attracted immune cells called macrophages to the gut. They then emitted free radicals that harmed the gut neurons responsible for gut motility – impairing that critical function.
Because the rate at which food substances pass through the gut affects the gut microflora, having low gut motility (constipation) or high gut motility (diarrhea) promotes harmful gut microflora growth. It’s possible that HSV-1 activated macrophages could be damaging and setting off nerves across the central nervous system.
Results
As noted earlier, the study assessed the presence of pathogens in the red streaks found in the biopsies of the gut lining. HSV-1 DNA was detected in the biopsies of 100% of the FM patients with gut issues, 80% of the people with gut issues but not FM, and 27% of the people who were being assessed for something other than a functional gut disorder. Despite the fact that other herpesviruses are known to infect the gut lining, no other herpesviruses were found.
The authors reported that the virus was active; i.e. it was replicating and pumping out infectious forms of the virus. They noted that HSV-1 is a potent virus, which, because it’s able to spread from synapse to synapse in the neurons, could be involved in many forms of FGID. Indeed, HSV-1 is able to establish infection both in sympathetic and parasympathetic nerves leading to the gut, and in the complex nervous system (enteric nervous system) found in the gut itself that affects gut motility, digestive secretion, blood flows, etc.

Carole Duffy led the study and Skip Pridgen started the whole thing off.
The authors noted that the study was small and that corroborating serological (antibody) data needed to be gathered. They called for much larger studies to assess the intriguing connection between HSV-1, fibromyalgia, and other functional gastrointestinal disorders.
This is the first study in years, if at all, to find replicating herpesviruses in fibromyalgia, and, of course, adds HSV-1 to the list of herpesviruses to consider in ME/CFS (Pridgen believes a similar situation exists in that disease). Plus, it suggests HSV-1 may play a role in functional gut issues in people who don’t have FM.
Correlation, of course, isn’t causation. Because the study examined people with FM with gut issues, it may not reflect what’s going on in people with FM who don’t have those issues. Pridgen reported, though, that most FM patients in his experience met the criteria for being in this study, and he finds red streaks in about 85% of FM patients he does endoscopies in.
Simply finding these strange herpes viruses littering the gut tissues of FM patients is a significant finding. Since the virus can travel from nerve to nerve one wonders where else in the body it may be present. The fact that it lives in the sensory nerves suggests it could be causing all manner of strange symptoms – and strange symptoms – as anyone knows who has these diseases – are a hallmark of them.
Pridgen believes the virus may be present in the trigeminal ganglia in the head and neck, the nodose ganglia in the GI tract, the dorsal root ganglia near the spine which transfer sensory signals from across the body into the spinal cord, and less commonly, the brain. The possibility the virus is producing some pretty dramatic symptoms certainly seems present.
It makes one wonder just what is hiding out in the tissues of people with ME/CFS, and one would hope it will prompt similar studies. Are those red streaks present in ME/CFS patients’ guts as well? If they’re present in people with “functional gastrointestinal disorders” (which includes IBS) one would suspect they would be present in at least some people with ME/CFS as well.
We’ll know more about Pridgen’s effort to eliminate these viruses in FM when Virios’s big FORTRESS study winds up. Perhaps because he’s founded what looks like a pretty formidable company, Pridgen’s FORTRESS trial seems to be on track – a rarity in ME/CFS. Results from the 400+ person phase II FM trial of Virios’ famvir/celexicob combination should be available by September.
Virios is also beginning a trial of a formulation of valacyclovir/celexicob in long COVID with Dr. Lucinda Bateman at the Bateman Horne Center in Salt Lake City, Utah. Pridgen has stated he plans to move forward on drug trials in ME/CFS as well. We may see that pattern – drug trials moving from FM to ME/CFS – more often as the interest in FM moves more towards the immune system.
Find out more about ongoing fibromyalgia clinical trials including some possible game-changers here.
Keep the News Coming! Support Health Rising!

It’s been a long road. Health Rising has kept you abreast of Dr. Pridgen’s work every step of the way.
With Pridgen’s 10-year effort antiviral effort in FM culminating in a couple of months, it’s an exciting time. If you heard about Dr. Pridgen’s work you probably heard about it via Health Rising. Why? Because over the past 8 years from a blog recounting an amazing recovery story using Pridgen’s protocol to updates on his progress we’ve produced a dozen blogs covering every step of the way.
Our commitment to you is to keep you abreast of every effort to improve the lives of people with FM, ME/CFS, and long COVID. If that’s important to you, please support us in a way that works for you. We are almost entirely community-supported.






I have ME/CFS and Fibromyalgia and have never had HSV-1 according to blood testing. I wonder if there are different types of HSV-1 testing? I had mine done at QUEST HSV1 1GG type specific AB.
Great question. I have no idea about antibody results. The authors simply stated they needed to be assessed. Hopefully, someone will know more.
~30% of the study patients who tested positive for HSV-1 by biopsy actually tested negative with a blood test. Blood test for HSV-1 IgG is not particularly accurate. Remember that the virus moves about through the nervous system.
👍🏼. Thank you, Dr. Prigden.
Several people in my family suffer from FMS /Myofascial Pain Syndrome. In recent years, a younger whipper snapper physical therapist said it was policy to read a book on fibromyalgia to his patients. I found it highly insulting and a reframe of the old philosophy that “It is all in your head.”, instead saying “Your brain is lying to you.” He even went so far as to say a groin pain I was experiencing was not a mechanical problem, ….. and later my PT said it was an iliac issue. It feels like the insurance companies are intent on brainwashing us.
Having this viral information is SOoo important to the mental health of everyone suffering from FMS. It makes so much more sense than hysteria and “lying brains”. Please press forward with the research.
It could be chemicals exposure as well, since I come from a farming family… Or, it could be plastics…. But, whatever it is, …. it is not a figment of our imaginations, and I want to blast this in the faces of all brainwashed doctors and P.T.s who are still harming people with this twisted narrative.
Terri
On behalf of the medical profession, I apologize for your unfortunate treatment to date. I would be happy to help you . Email me at tsasurgery@gmail.com
what about the enteroviruses, found by doctor Chia? And all other herpes viruses. It is clear that the immune system of ME/FM/POTS/IBS patients cannot control these infections. These should be switched off and go to ‘sleep’. Behind this lies the cause of these diseases.
Many more biopsies of other organs should be performed on these patient groups. And after death also the brain, spinal cord, heart and circulatory system.
Just wondering if anyone else loses their taste and/or smell during viral reactivation?
I was diagnosed with ME/CFS over 20 plus years ago….I believe it all began after severe case of VZV (chicken pox) in high school.
Since that time, I intermittently completely lose all sense of taste
(Ageusia). I have not had covid, which Loss of taste/smell has been one of the symptoms.
Fortunately, my taste will return, longest time frame without taste was three months!
I also experience intermittent shingles…I do take famvir which seems to keep the shingle recurrences at bay. No benefit with energy
Or overall symptoms with famvir, however.
Just curious if Dr. Pridgen
Sees this in any of his patients?
during my acute stage of my viral infection I’ve had gut issues. Sometimes when i feel a stool moving in my gut i have very unpleasant neural sensations occurring in my pelvis. No GI consultant can explain what causes this. I now frequently get cold sores that become infected with bacteria. So, I know i have Herpes Simplex 1 in my body.
I hope this work helps us.
This is a great study and I’ve always wondered if my HSV-1 had any correlation with my fibromyalgia especially when I get a cold sore! I’ve started a regimen of acyclovir everyday 3x daily. I want to see if that will affect my consistent fibromyalgia pain which never stops but moves from different areas of my body. The only thing that comes close to touching my pain to ease it in anyway is Kratom. I’ve been on that for two years now & at least I can get out of bed & function at my job & life in general. Is anyone here experiencing long Covid bcuz I had a fever for a week straight while having Covid & now I’m dealing with even more fibromyalgia flares. My thoracic back pain has been off the charts & it was terrible while I had Covid with no real Covid symptoms just the constant fever with a little congestion, no loss of smell or taste. I’ve also lost 50% of my hair and I’m 7 months post my Covid diagnosis. It’s studies like these that give me hope of potentially understanding this horrible disease so thank u!
I am so glad I read this article! Me as well I’m 7 months post Covid. My back gave me fits and I had a slight fever. Ever since then my fibromyalgia has been at its worse. Not being able to function at work just trying to push through barely. Always having to complain and I absolutely hate that. Doctors looking at you like you don’t know what your talking about. I haven’t heard of Kraton before but I am going to look into it. Thank you for the information!!
I should have added, I do have gut issues, so if this theory is valid, why am I not testing positive to HSV-1?
More information on antibodies – https://www.webmd.com/genital-herpes/what-is-herpes-simplex-virus-antibodies-test. The IgM test is not recommended.
The antibody tests assess a past infection – and a lot of people carry HSV-1 or 2. These tests are not infallible as some people don’t produce many antibodies. I know someone with ME/CFS who regularly tests positive for a CMV infection but doesn’t test positive for EBV – which doesn’t make sense given how much more prevalent EBV is. On the other hand, maybe you’ve never been exposed to it, and something else is causing the gut troubles.
The standard test for an active HSV-1 infection is a PCR test.
Hi I have had recurrent outbreaks of herpes simplex since I was 21 and then developed CFS in my 40s and fibromyalgia in my 50s. I discovered by myself that if I took 2000 mgs of valtrex every day I could keep most of the symptoms under control. I also had bad gut issues until I started making home made kefir, which dramatically improved my fybro symptoms. So this study is the first I have seen that makes sense of all this. Have had virtually no help from GPS have worked it all out alone.
Interesting about the homemade kefir as I find it is so much more powerful than the store-bought kind that they are hardly comparable. We have a story of one person who recovered using fermented foods and fasting.
Catherine, would you share your homemade kefir recipe?
A few years ago, a research study was published finding HSV1 has mutated over the centuries like other viruses do, and a strain exists that learned to not break through the skin where Oxygen can kill it, but to travel the other direction along the nerve deeper inside the body. So people who have never had a breakout may still have HSV1 causing internal nerve pain and damage.
Oh, cort. Another avenue. Hoping this one in the ONE. THANK YOU TO DR. SKIP AND CAROLE. I WILL BE SO ANXIOUS TO SEE SEPT RESULTS. WHAT A MIRACLE IT WOULD BE IF THIS WAS “it”. It has been a long long long time to feel so bad everyday. Sincerely, Javen
Hi Cort, do you have any idea of the dosages that Virios is using for their valacyclovir/celexicob trial?
I have both in the cupboard and would like to see if increasing the valacyclovir will help…
I’m afraid I don’t. I looked for it in the clinicaltrials.gov database but was unable to find it.
Kudos, Cort, for your hard work keeping relevant work front and centre, such as Skip Pridgen MD and Carole Duffy‘s work.
I clicked on your “possible game-changers here” link that led to article with this link:
https://www.clinicaltrials.gov/
Took a brief look and was discouraged to see
CBT
and
LIGHTENING PROCESS
listed in trials.
This article brought me to tears. I’ve had HSV 2 (with possible HSV1 coinfection) for 45 years. I’ve struggled with gastric issues all this time, and it’s only gotten worse since an organ transplant.
I have FM, CFS and now chronic gastritis. I suspected HSV was the culprit because the gastritis started at the same time as a huge outbreak AND trigemenal nerve pain! I have an endoscopy in June and I’m really hoping they confirm the presence of HSV so treatment will be prescribed. As an immunocompromised person, it scares me to think what this nasty virus is doing to my body.
Peggi, I have had fm cfs for around 20 years with IBS. I. Have been on celecoxib for at least 10 of those years and 4 years ago I started being treated with acyclovir for herpes simplex 1. My IBS has almost completely gone. I thought it was digestive advantage for intensive bowel treatment that was helping it. Maybe it’s been both!
Interesting thanks Cort. Many IBS are misdiagnosed when they actually have Sibo -small intestinal bacterial overgrowth. I was one of them. What a relief it was to find I could treat it. Sadly no cure as it re occurs especially if you don’t do a very low carb diet.
Glad to hear it helped Linda! Dr, Chedda reported it was very common in these diseases – but I don’t think we hear nearly enough about it.
https://www.healthrising.org/blog/2019/08/26/bela-chedda-chronic-fatigue-syndrome-center-complex-diseases/
Health Rising does have several blogs on it.
From the Gut to the Brain: Esther’s Amazing Chronic Fatigue Syndrome Xifaxin Story – https://www.healthrising.org/blog/2014/06/06/gut-brain-esthers-chronic-fatigue-syndrome-xifaxin-story/
Diet, Drugs, Herbs and SIBO: One ME/CFS/FM Patient Finds Relief with the Pimental Approach
https://www.healthrising.org/blog/2014/07/25/diet-drugs-herbs-sibo-one-patients-experience-pimental-approach/
Cheaper, Safer, Better: the Herbal Approach To Small Intestinal Bacterial Overgrowth
https://www.healthrising.org/blog/2014/06/25/cheaper-safer-better-herbal-approach-small-intestinal-bacterial-overgrowth/
but nothing for quite awhile.
Were you able to resolve it via diet or did you do something else as well?
Have you tried spore-based probiotics to rehabilitate the microbiome?
After many years of serious IBS (and M.E/CFS) and taking conventional probiotics to no avail, I moved over to the more recently developed spore-based probiotics with almost miraculous results.
Unfortunately not doing so well on the M.E. front, but I was until COVID-19 got me and knocked me back a few years.
I know that after I’ve been sick, I’ll inevitably break out with a cold sore on my lip. This have been with me most of my life and I’ve wondered if it’s somehow involved with ME.
Same with me.
I get a cold sore when I’m in a me/cfs flare. I’ve tested positive for HSV1 + 6 and I take valtrex daily.
Hi I got diagnosed with m.e and fibro 11 years ago.. 4 years into my sickness I went to a specialist, where I was given multiple blood tests.. When my results came back it showed my I had herpes.. I had suffered with coldsores for many years prior to getting m.e.. Plus many years of hell with mouth ulcers.. The difference in 2010 was I had a very big break out of herpes on my lips and mouth… This continued for many years.. Until a different gp from my own who completely dropped the ball… Said these are not mouth ulcers they are coldsores in your mouth herpes.. I started off on zovorx tablets.. Then they didn’t work.. Now I take valiciclovir daily 500mg..if they are really bad I also use predislone and its very helpful… Not sure if this information is any use.. But it was my journey..
H.M
My mother most of her life had cold sore in her mouth that she said were herpes. She lived till she was 85 and use to tell people she walked 2 miles every day. Actually it was every other day but with Alzheimer’s in the last 10 years, bless her heart she couldn’t remember. My father on the other hand , I am almost positive had fm. I used to watch him go up and down a small set of stairs and could literally feel his pain. Thank you Cort for all you do. The red ginseng from dr. Teitelbaum has helped my cfs tremendously too. Praise the Lord!!
Thanks for another great article Cort. Very timely. I spent much of today reading up on dorsal root/sensory and autonomic ganglionitis, and it’s links to both HSV-1 and VZV infection. Ganglionitis of the sensory neurons has been found in the autopsies of a few ME patients. And both of these infections like to reside in the dorsal root ganglia in particular. I hadn’t realised that only HSV-1 can infect the gut neurons so that’s very interesting. I’ve been researching it from the perspective of Sjögren’s syndrome and non-length dependent neuropathy in Sjogrens, which is often mislabelled as fibromyalgia. Ganglionitis of the dorsal root (sensory spinal neurons) has been shown in sjogrens. Between that similar pain manifestation (allodynia, positive sensory symptoms) , and the overlap in severe fatigue of SS, I’m beginning to wonder if some subtypes of ME, FM and SS are a continuum rather than discrete illnesses. Or at least can have substantial overlap possibly in causality as well as symptom presentation. There have also been those recent findings of IgG antibodies in patients with fibromyalgia (the mouse study) where these antibodies were found to bind to the satellite glial cells of the dorsal root ganglia. So hard not to think that viruses, the ganglia, and aberrant immune responses are not heavily involved in at least a subset of FM/SS patients. And a further study comes to mind a few years ago that found anti-calponin 3 antibodies in SS patients, which also were shown to bind in particular to the satellite glial cells of the DRG. Pesky viruses residing there, whether latent or active seem to be problematic for some of us! Thanks again for publishing
So interesting Debbie! I have been wondering about the Sjogren’s Syndrome (SS) connection since hearing Lauren Stile’s story. She never tested positive for SS until she had a lip biopsy done – and that was it.
https://www.healthrising.org/blog/2013/08/20/from-chronic-fatigue-syndrome-to-fibromyalgia-to-pots-to-success-one-womans-journey-through-the-medical-profession/
Brent Goodman talked about how under-diagnosed SS was in POTS – and I imagine it’s true in ME/CFS as well. He believes that “A diagnosis of Sjögren Syndrome should be aggressively pursued in patients with signs and symptoms suggestive of autonomic nervous system impairment.”
He also said “if you can think of a neurological condition Sjogren’s Syndrome can cause it“.
My mother had a terrible bout of Sjogren’s Syndrome. And now you bring up a connection between the kind of small fiber neuropathy found in Sjogren’s and FM.
Fascinating! Thanks 🙂
Dear everyone, may I suggest to spell out abbreviations when used for the first time so we can all understand and keep learning? I eventually deduced SS probably means Sjogren’s syndrome but it is difficult to understand articles with cognitive issues as it is, so no cryptic abbreviations is much appreciated 🙂 Thanks!
I will remember to do that. Debbie did use SS in connection with Sjogren’s and I did as well but did not explicitly link the abbreviation to the condition. I always try to do that in the blogs but could have done better in the comments. Thanks for the reminder. (I’m fixing my comment now – I have the ability to do that :))
I’m very sorry to hear that your mother suffered that too, I can relate.
Yes, I often now wonder if fibromyalgia is ‘basically’ non length dependent small fibre neuropathy (possibly without reduced nerve fibre density due to regrowth), caused by immune attack on the dorsal root ganglia (DRG) /satellite glial cells (SCG), perhaps in response to a pathogen residing in the DRG. This could be caused by Sjogrens, or no doubt other immune dysfunction. Not to mention a latent pathogen itself perhaps setting off signals/attempting to reactivate.
I’m also now wondering how this relates to the findings explained and summarised in your other recent article, that natural killer (NK) cells are attacking sensory nerve fibres in response to some signal they (or the scg or drg) are releasing. How does this relate to what is happening with the autoantibodies found binding to the satellite glial cells of the DRG? So many interesting questions here. I hope these different research groups are talking to one another. Seems like they could make major breakthroughs working together in cooperation!
Thanks again for keeping us informed!
I’ve had a ME diagnosis since the 80’s and a FM diagnosis since the 90’s. I developed quite severe sensory neuronopathy last year, directly after an episode of gastritis. I had low grade fever for months, lost lots of hair and developed an extremely dry mouth and spine pain. So now I have the Sjogrens diagnosis on top! Well in my case anyway, these conditions do seem to overlap. :/
I’m going to check out those links you’ve provided. Thanks so much. x
Apologies JR and all for the use of shorthand/abbreviations, a bad habit I’m trying to get out of! It was a bit of an unfiltered brain dump on my part in response to the article, it just sparked so many interesting thoughts!
I have had severe MECFS & Fibromyalgia for 22 years. I also have “Shingles” outbreaks on my left hip, left thigh and the area around the left side of my iliac crest. I have also had 7 serious spine surgeries since childhood. No Doctor has ever been interested in the fact that I have recurrent Shingles. No one has suggested this was sexually contracted herpes. The area is typically as big as a small apple. (Larger than typical herpes blisters and smaller than typical Shingles outbreaks).
These outbreaks typically happen when I am under extreme pain, extreme emotional stress or an extreme physical illness such as Pneumonia.
Can my physician test these outbreaks? If so, how and why do I convince her to do so? What would I do with the results?
Thanks
Seems their is definitely a problem with the detection of these viruses in normal serology tests. Maybe the best approach is to treat the same as for HIV and AIDS which would stop the replication of whichever active Herpes viruses the person has. With HIV the virus replication is stopped with a combination of antiviral medications. The new treatments being tested for HIV are monoclonal antibodies and may also be helpful for M/E CFS and Long COVID and all autoimmune diseases.
Dennis – I have seen so much recent research showing a connection here.
I read one study documenting use of anti-retrovirals in MS controlling EBV infections in a one off study, they also stated that the more common antiviral drugs (like those Pridgen is using) do NOT control EBV.
Also, Dr. Bruce Patterson frequently uses the CCR5 Antagonist Maraviroc in treating Long COVID patients.
I think that the testing being used obviously misses reactivation as well. This leaves the question as to WHY this happens to people when others can control these viruses and keep them latent.
The addition of Celebrex to valacyclovir probably renders valacyclovir effective against EBV. It blocks the COX-1 and 2 enzymes which are needed to produce new VIRION’s and it breaks apart the outer membrane of the viruses making them susceptible to our immune system. The EBV does have Thymidine kinase which is needed to convert the antivirals to their active form. The Famvir dose would likely be around 1.5 g a day and the dose of valacyclovir would likely need to be 3 g a day. There are more and more instances of synergy in recent meds showing that combinations of meds can do what single meds can’t. See HIV, Hep B and C and new cancer drugs.
renders valacyclovir effective against EBV. It blocks the COX-1 & 2 enzymes which is needed to produce new virions
Thanks! It makes you wonder why doctors don’t go after synergies more often.
Reading the first paragraph I flashed to my childhood. Years & years of cold sores, shingles in my 20’s…makes a lot of sense. I’ve not taken meds for it, would be interested to see how my long term Fibro would respond.
Intriguing!
Daily Valtrex at 1000 mg has literally changed my life…3 years ago, I went from crushing, disabling relapsing and remitting CFS/ME continually (for close to 20 years) to high functioning return to quality of life. I work out almost daily, recently launched a part time business and parent two kids.
Without setting anyone off on overdosing on herbal substances, and noting I’m not a doctor… I’ve found in my family that olive leaf extract has a remarkable impact on herpes simplex virus, the type which creates cold sores. It helps if taken internally and (if you can stand the sting) topically. The quality matters and I had best results with a spray I bought from a homeopath, the brand was sevenpointfive, but others includng a tincture I made at home, were helpful too.
Here is an article corroborating the effectiveness.
https://www.sciencedirect.com/science/article/abs/pii/S1550830721000045#:~:text=The%20olive%20leaf%20extract%20has,impact%20against%20the%20various%20viruses.&text=The%20olive%20leaf%20extract%20was,in%20patients%20with%20HSV%2D1.
I have just done a quick search about the herb Andrographis having good antiviral activity against HSV 1 and I think it also has some antiviral activity against many other viruses including Sars Covid 19.
I have had a mild form of ME since 1979 after 2 weeks of flu but recovered my energy after about a year but was left with severe regualar vertigo attacks that were horrific followed by severe migraines both of which I felt I had no control and were very frightening, severely affecting my central nervous system and my ability to work full time.
Also I picked up so many viruses and infections during the 90s with the perimenopause finally pushing me into full blown ME./CFS. I have improved a little since the early 2000s with adrenal and thyroid and female hormone support but still very regularly have a virus that always starts in the same way with a sore throat to a greater or lesser degree, swollen gland under my left ear, a huge drop in my usual depleted energy and a feeling of being very unwell. Usually there will be an accompanying migraine.
However if I take Andrographis, around 4 large capsules daily, things will start to improve after a few days and if I am lucky I might get over it by day 4. Recently I even avoided getting Covid badly (or at all cos always negative) even though I had many of the symptoms for 3 days and was very unwell plus my partner who lives with me was very unwell with it for nearly 2 weeks.
I don’t have a clue what this persistent virus is that frequently reactivates but I did have a viral panel done around 10 years ago and it showed raised levels of 5 of the Herpes viruses including HSV 1.
Cort, doesn’t Whitney DaFoe take an antiviral?
I was severely ill for 6 years with ME. Bed ridden for 90% of the time and with nerve pain I still shudder to think of. If I’d had a gun I’d not be writing this now.
The ONLY person who got me well and showed me the path out of hell was Dr Skip Pridgen and his treatment. It’s not an overnight fix, you must stay with it and it took 7 months on the meds before I saw the changes. For many it takes 5 months. I’m still on the medication, almost 3 years now.
But it saved me. I now walk, play tennis, garden, bike and can think with working cognitive function back and the nerve body pain, the involuntary myclonic jerks wracking by body…gone. I will never forget that terrible evil place. So my message to all of you out there…do not give up!
What is that treatment can you please share?
While we’re waiting for the results of the Virios study, can you do an update on the use of herbs (and other dietary regimens)? You had some links to earlier studies, but they are several years old now. Anything new? At various points in my life I have tested positive for all 5 of the major herpes viruses, and have struggled with fatigue for 50-some years. I also have multiple autoimmune diseases, and I’d rather try more “natural” treatments first, resorting to drugs only as a last resort.
On another note, some of the research on long covid indicates some sort of connection with (either new or reactivated?) Epstein-Barr Virus. And after each of my 3 covid vaccine doses, I have experienced either a Herpes outbreak, or a Shingles outbreak, or both.
I have had CFS/Fibro for 36 years. The only treatment that has ever given me significant (virtually complete) relief from all of my symptoms was a regimen for H.Pylori (taken as a trial, even though I tested negative for H.Pylori). The regimen consisted of 2 weeks of Bismuth (Pepto Bismol) to which was then added Biaxin (Clarithromycin) and either tetracycline or minocycline, for 2 more weeks. During the first week of the abx I was unusually fatigued. Then during the second week, all of my symptoms resolved. It was incredible. I felt better (with more energy) than I remembered ever feeling in my lifetime. Unfortunately, all of my symptoms slowly returned again after I finished the regimen. This research and viral hypothesis rang the bell of this memory. I had always suspected a gut bacterial imbalance, but diets to manage the microbiome have been to no avail. This research suggests that perhaps viruses may be responsible or implicated. A quick search just told me that Bismuth also has anti-viral properties, and so might Clarithromycin (as one of the macrolides – some of which seem to help with Covid). My personal experience seems to support this research’s viral findings. I have tried many hundreds of treatments – almost anything that might have helped (without danger) from both conventional and alternative medicine supplements. Nothing else even came close to the total recovery of this 3 component H.Pylori trial. Thus, I hope there is more research in this direction.
I have ulcerative colitis , diagnosed at 24 and now in remission with meds, 50 years later. Then fibro diagnosed at 54, but with first symptoms in early 40’s. That is controlled with major life style changes, physical therapy, and meds. Never had a cold sore ever that I remember. So, I read your article with fascination. Will more clinical trials be done? How can I sign up for one?
I want to know if the herpes simplex virus and macrophages could cause gut permeability that predisposes people to food allergies.
I know I tested positive for Herpes simplex. I just have to wonder why my immune system started freaking out about food like it was an invader.
Maybe the immune system was hyped up from herpes simplex. Does that sound plausible to anyone?
I had herpes simplex 1 outbreaks, as a child, every single time I ate a little bit of cheese (doc said it was an allergy).
But here is where it gets interesting. As a child, I always drank milk, with no issues. Now as an adult, that is flipped…I have horrible time with milk, but cheese causes me no issues. How strange is that. For me…herpes is related to allergies.
39 years suffering with FM/ME/CFS. I got ill right after the birth of my 2nd (out of 3) child
I am post menopausal now, but always had herpes breakouts during menstrual cycle. Doc gave my Acyclovir and it helped dramatically. I always had way worse FM/ME/CFS symptoms in my menstrual years occuring in sequence with menstruation…with hardly any symptoms during my pregnancies. Now that I am post menopausal, again my symptoms are lesser. I used to be bedridden. Now I can get out a couple times a week, providing I keep a very low stress level during outings (I use a wheelchair to lessen too much walking/standing stress).
I have some questions:
1. Is Acyclovir similar to Valcyclovir?
If so, should I ask Doctor to give me Valcyclovir instead of Acyclovir for symptoms? I thought valcyclovir was only used for herpes 2 (genital)?
2. Does FM/ME/CFS get worse during menstrual cycle for most women?
3. Are menstrual cycle hormones complicit on body to create triggers?
Thanx…looking forward to input 🙂
I had constant cold sores while on my period. Now I’m in menopause & I get them more often it seems. I too take acyclovir for cold sores & I’ve upped my dosage to 3x daily to stave off the constant cold sores. I’ve always wondered if my fibromyalgia had some correlation with my HSV1 diagnosis. Now I’ve started getting internal mouth sores, patchy white spots that peel, eating is somewhat difficult during these flares that occur. I’m also curious if I need to change my acyclovir to valacyclovir! It sounds like it could be a game changer with fibromyalgia and of course while treating my HSV1!
I had herpes simplex 1 outbreaks, as a child, every single time I ate a little bit of cheese (doc said it was an allergy).
But here is where it gets interesting. As a child, I always drank milk, with no issues. Now as an adult, that is flipped…I have horrible time with milk, but cheese causes me no issues. How strange is that. For me…herpes is related to allergies.
I use Valcyclovir for Herpes Simplex 1 in my eye, taking 500mg 3X a day in addition to eye drops. My ME/CFS was triggered by Epstein Barr Virus (EBV) according to my titers 36 years ago. I took Valcyte under Dr. Montoya’s care when he did his study. I was put on Xifaxan to treat IBS-D probably 10 plus years ago and still take that. I also have Fibromyalgia. I’m currently dealing with terrible gastric symptoms. (There is a story here on Health Rising about my remission from ME/CFS symptoms when I first started Xifaxan.)
Dr. Pridgen, you were so kind when I spoke to you. Perhaps you recall a lady from Nashville. I’m wondering whether I should increase my valcyclovir and add the additional anti-viral? I always assumed that the valcyclovir I was using for my eye would be treating EBV at my current dosage. Are you still seeing patients and would my case be helpful to your research?
After reading this article and about Dr. Pridgen’s research, I immediately went to my doctor and got prescribed Famvir and Celebrex. I have had fibromyalgia for over 30 years. I have been on Famvir and Celebrex for two weeks now, and do not notice any improvement. I am thinking it is because I have had fibromyalgia for so long that it may take awhile. I know the research stated that it was after 3 months of being on the protocol that patients felt better. However, it also stated that people had sporadic improvements during and up to that 3 month period. Has anyone else started taking this drug combination and if so, when did you start feeling less pain?
When I read about this study on your blog, I immediately went to my MD to as if she would put me/ (us my wife, too) on famciclovir and celecoxib. She read the study and agreed. We have been taking the combination a little less than a month. My energy level has gone through the roof. I’m sleeping and eating better. My wife has improved somewhat but not as well as me. Plus, she’s having strange side effects, such as a burning mouth, tingling in both arms, headache, and nausea. I have no side effects so far. She stopped taking the medication and will begin taking celecoxib in a few days to see how she does. Then maybe a smaller dose of famciclovir. We also take xifaxan and drink homemade kifer we make with raw milk daily.
I have both HSV 1 & 2 and I started feeling symptoms of FM about 1 month after contracting both viruses at the same time. I also started experiencing guy problems around the same time. So now I have HSV 1&2 along with FM/CFS and IBS. This has destroyed my life and I pray that these trials are successful. So many people are suffering with FM/CFS/IBS. I truly believe there is a link between these disorders and the herpes virus. I was 50 years old when this all started and I was perfectly healthy. It all went downhill within 6 months of contracting herpes.
We have very similar stories. It’s absolutely awful isn’t it. Like you I was so strong , fit and healthy just being all of this. Try telling your doctor or sexual health clinic you are having persistent break outs and they may put you on a 3 month course to make it dormant again. I struggled to take the pills and having no idea that it was effecting my FM I didn’t complete the course. I share as hell will now though!! And ask for more. Good luck my love. Sending you much strength and positivity
I found this article because after 2 years I have finally seen without a doubt that my fibro flares up badly two weeks prior to a herpes breakout, literally just before the blisters appear my FM symptoms start to subside. I thought there had to be something in this. Plus since being put on an intensive course of tablets for 3 months for the virus my symptoms have improved.
Also my gut is the baine of my life. When I went for an endoscopy I saw the red streaks myself on the camera. Yet nobody said a word about what they could be.
I’m going to go back to ask my doctor for another 3 month course and if I see the same improvement then it’s undoubtedly the answer to the hell I have been living for the past 4 years . I have had herpes for over 20 years and it didn’t give me much bother. Around the time of my first Covid jab all these pains started and the virus kicked up its ugly head again. I also lost my parent that year so all the medical professionals are putting it on that . But I have never really believed that to be true as I was already undergoing tests before he died. This makes more sense that anything I have researched over the past 4 years
Hi Dr Pridgen,
This is the case with me but I only have Hsv2 my symptoms lasts for weeks and soon as I take anti virals (valtrex) all my joint pain disappear. However if I don’t take it longer it can come back. I don’t have ME but they diagnosed me with “FM” which I didnt want to accept as I knew there is something that’s causing this pain and it felt like my body was reacting to something. All blood tests coming back fine apart from a low neutrophil count while I was ill with the pains, until I was better then they go back to normal. So this was telling me that it was a viral and that you were correct in your study. I don’t like taking the antivirals long term because I worry about side affects?
Have you ever had c3 c4 tested
Hi, I think ANA tests I’ve had a couple of times RA factor and CRP tests and nothing!! Only a Low neutrophil count when I’ve been ill and had bloods done at that time. I thought I had lupus but with them tests coming back neg I thought it can’t be that. I really don’t buy the fibromyalgia for me. I’m currently in pain in joints, not to walk or touch just painful inside it’s like I’m ill with a virus, ill randomly get better after some weeks have a a couple weeks being totally pain free then bang it hits me again.