

Therefore many patients without tachycardia remain undiagnosed by the tilt test if the end tidal CO2 and CBFv are not measured. Novak – author
Orthostatic intolerance just got a bit more complex. That was actually good news. Hopefully chronic fatigue syndrome (ME/CFS) will soon get more complex in the same way.
Usually when we think of problems standing or orthostatic intolerance (OI) we think about postural orthostatic tachycardia syndrome (POTS), which is characterized by a greatly increased heart rate upon standing. There’s also, less commonly, orthostatic hypotension (low blood pressure upon standing).
Both disorders produce similar symptoms (lightheadedness, dizziness, headache, nausea, fatigue, shortness of breath) upon standing that are relieved by lying down. Both also feature sympathetic nervous system hyperactivity and reduced blood flow to the brain (cerebral hypoperfusion).
But neither condition describes everyone. Dr. Peter Novak, Chief of the Autonomic Neurology Division within the Department of Neurology at Brigham and Women’s Hospital in Boston knew there was more to the OI story than was meeting the eye. He had plenty of patients with orthostatic intolerance (problems standing without having symptoms), which didn’t fit into either of those categories. He decided to dig deeper, and when he did, he uncovered what appears to be a new kind of OI.
Novak P (2018) Hypocapnic cerebral hypoperfusion: A biomarker of orthostatic intolerance. PLoS ONE 13(9): e0204419. https://doi.org/10.1371/journal.pone.0204419
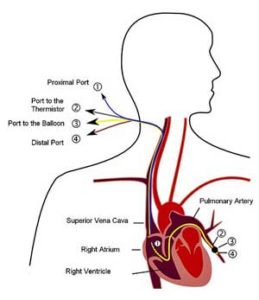
Novak found this group by putting patients with orthostatic intolerance but without POTS or blood pressure problems (or ME/CFS or fibromyalgia for that matter) through tilt table tests while measuring their CO2 levels and blood flow to the brain.
He discovered that these mystery patients had something called hypocapnic cerebral hypoperfusion; i.e., upon being tilted they were emitting abnormally low levels of carbon dioxide (CO2) and had disturbingly low blood flow to the brain.
Hypocapnia or low CO2 levels are not new to orthostatic intolerance; low CO2 levels appear to be common in POTS, for instance, but no one had uncovered a group of OI patients who only had hypocapnia.
Low CO2 levels are often associated with deep breathing or hyperventilation syndrome – a tricky diagnosis. Hyperventilation is divided into two types – secondary (caused by physiological factors) or primary (caused by psychological factors such as anxiety). The MERCK Manual focuses almost entirely on primary hyperventilation.

The new group had low levels of CO2 and low blood flows to the brain but no increases in heart rate or drops in blood pressure.
Novak did everything he could to knock out the physiological factors group by preventing anyone with a disorder/problem that could cause hyperventilation (lung disorders, low blood pressure, severe metabolic abnormalities, central nervous system disorders (FM, ME/CFS), drugs and high amounts of pain) from participating in the study.
That would seem to leave anxiety as the only remaining cause of OI for this group, but that wasn’t the case. The field is so unexplored that Novak couldn’t come to any conclusions about what caused the low CO2 levels he’d seen.
He did, however, come up with a rather long list of possibilities, including baroreceptor problems interfering with “respiratory drive” compensation for metabolic acidosis, orthostatic ventilation-perfusion mismatch, problems with the respiratory centers in the brain and others…
Under the Radar No More
This group of patients, which appears to be fairly common, has apparently gone under the radar for years. Novak noted that more than 80% of the patients in this study had been referred to him as suspected POTS patients. Most doctors would have likely given them a tilt table test, found no evidence of POTS, and sent them on their way.
Novak reminds me of his colleague, pulmonologist David Systrom, who, while working at the same hospital, gave patients with idiopathic (i.e. unexplained) exercise intolerance (including people with ME/CFS, POTS) a deeper look. These people, also not uncommon, had passed fruitlessly through the medical system for years. Systrom decided to use his invasive cardiopulmonary testing to examine them in detail, and uncovered a fascinating group of patients.
Next, Novak will try to differentiate these groups further and determine if hypocapnic cerebral hypoperfusion is commonly found in POTS, and whether it is an entirely different disease or exists on a spectrum of orthostatic intolerance disorders.
The central takeaway from this study is that if you have problems standing, and have been tested for OI and been found wanting because you didn’t display a high heart rate or a drop in blood pressure, an end-tidal CO2 test might be the test for you.
If that’s so, you should tell your doctor that low CO2 levels have been linked to low blood flow to the brain in OI. Low CO2 levels have been found in ME/CFS and FM dating back to 2007 and 2010. In fact, ME/CFS and FM were two of the three diseases that Novak reported exhibited hypocapnic hypoperfusion in his paper.
- Check out how to do an in-home test for hypocapnic hyperventilation – A Home Postural Hypocapnic Hyperventilation Test for Chronic Fatigue Syndrome and Fibromyalgia
Core Feature Identified
Novak noted that the “spectrum of orthostatic intolerance is broad, complicated, and includes several overlapping presentations”, but one factor, thus far, links them together. So far, every form of OI, including hypocapnic cerebral hypoperfusion, has had one thing in common – a decrease in blood flow to the brain while standing. Problems getting proper blood flow to the brain may be the core feature of all these forms of orthostatic intolerance.
That, interestingly, was the same conclusion Dr. David Bell came to almost twenty years ago in chronic fatigue syndrome (ME/CFS).
The Brain Blood Flow Problem in ME/CFS #1: Maggie’s Story
Her panic was organic in nature; it came on as a result of physiologic, not psychiatric, factors. Dr. David Bell
Almost twenty years ago Dr. Bell concluded that people with ME/CFS were having trouble getting blood to the brain. He explained his thinking in a vivid example, republished on Health Rising as “When Panic Isn’t: Dr. Bell on Maggie’s ME/CFS and Fibromyalgia Story“.
Maggie had been doggedly looking for an answer to health problems for ten years when she met up with Dr. Bell. She’d repeatedly been diagnosed with panic disorder, but the exhaustion she felt, her cognitive problems, her leaden feeling legs, etc. didn’t signal panic to him at all. They signaled ME/CFS.
Blood volume and standing tests revealed real physiological abnormalities. Maggie was fine until about the ten-minute mark of her standing test when she began experiencing fatigue, pain, lightheadedness and a feeling of panic. At that point her heart rate, blood pressure and epinephrine (adrenaline) levels shot up. She was diagnosed with hyperadrenergic POTS, low blood volume, orthostatic diastolic hypertension, as well as ME/CFS and FM.
“Whatever else this disease does to the human brain, it includes agitation in its repertoire.” Dr. David Bell
We don’t know if Maggie also had hypocapnia, but it doesn’t matter. Her panicked feeling was probably the result of her epinephrine levels going bananas in an attempt to get more blood to her brain. In the end, Bell felt that some form of panic or agitation was a core part of ME/CFS, but it was not a psychological problem – it was the result of low brain blood levels – the same core problem Novak found in his hypocapnic patients who did not have ME/CFS or FM.
The Brain Blood Flow Problem in ME/CFS Fixed – Temporarily…
A fascinating study also suggested that reduced blood flows to the brain is perhaps the key issue for one group of ME/CFS patients. When researchers were able to temporarily fix that issue their symptoms completely disappeared.
This group of younger ME/CFS patients looked quite normal lying down, but tilting them up sent their systems haywire. Relative to the healthy controls, their heart and breathing rates increased by about 50%, their CO2 levels dropped by 25%, and they experienced a 50% drop in blood flow to the brain. Not surprisingly, their cognitive performance also dropped dramatically.
Remarkably, phenylephrine, a blood vessel constrictor, returned brain blood flows to normal and removed the symptoms of one group of ME/CFS patients.
Remarkably, all those symptoms were reversed with the administration of phenylephrine. The ME/CFS patients’ cardiovascular and cognitive test results normalized leaving them looking like healthy controls. The authors believed phenylephrine fixed the central problem in this group of patients – reduced blood flow to the brain.
Phenylephrine causes the blood vessels, interestingly, to narrow (vasoconstrict). Its success suggested that either not enough blood was flowing to the brain and/or inflammation was dilating the blood vessels. Either way the pressure needed to move their blood into smaller blood vessels was missing.
Phenylephrine, interestingly, is often used in hospitals to increase blood pressure and reduce the vasodilating (blood vessel opening) effects of systemic inflammation and sepsis. That’s an interesting finding, given the possibility that ME/CFS may be an atypical form of sepsis – something Dr. David Bell also suggested years ago.
Dr. Stewart, the author of that study, believed that finding ways to get more blood into the brain was going to be key in this group of patients. (Unfortunately the inhaled form of phenylephrine does not work.)
Wrap-Up
Novak’s identification of new kind of orthostatic intolerance suggests that the deeper researchers dig the more there is to find. They also, suggest, though, that all kinds of OI may link back to one central problem – the inability to get sufficient amounts of blood to the brain. Stewart’s study suggests that the same core problem is afflicting at least one subset of ME/CFS patients.
They also suggest that some of the problems found in ME/CFS/FM are not unique to it. Novak’s experience was similar to David Systrom who found that a whole raft of patients (ME/CFS, FM, POTS and others) had problems with preload or mitochondrial functioning which impaired their ability to exercise.
Interestingly, by reducing blood flows to the heart, the preload problems Systrom found could conceivably affect blood flows to the brain. Dr. Shungu’s brain lactate findings, the reduced blood volume in ME/CFS, and Ron Davis’s red blood cell studies are adding other blood flow elements into the picture.
Since those studies have not been done in Novak’s or Systrom’s patients, we don’t know if those findings apply to them, but it’s looking more and more like some of the core issues involving blood flows and blood vessels occurring in ME/CFS are probably occurring in other diseases. Given how terribly debilitating ME/CFS, in particular, can be, it makes sense that it’s impacting very basic physiological processes. Ron Davis has repeatedly stated that he believes understanding ME/CFS will accelerate our understanding of other diseases.
So did Dr. Bell almost twenty years ago.
CFS, and the patients who suffer from it, have a great deal to teach those of us who have made medicine our life. Once researchers unravel the physiologic mechanisms of this illness, the discoveries will help unravel basic mechanisms of unnumbered other diseases.








Does it make sense in regards to these findings that a CFS/FM sufferer feels significantly better during pregnancy because of increased blood flow?
I have the same Experience. I was Able to Walk on High heels when pregnant, which wasn’t possible for many years before.
What?!!!!!
I felt so much better when pregnant, of course due to some of my other illnesses (only discovered recently, now 66)
I still had very strange things occurring in my blood/blood pressure/waterworks/hormones etc –
I had 5 children over 20yrs(one was an extended pregnancy as the 1st baby died & the 2nd conceived 3mth in was born with the placenta from the 1st baby)
I am sure having them saved my life due to the boost it gave me from the stem cells
I felt better when I was pregnant also. I also got pregnant with alarming ease. I had no idea how others might have felt during these times. It looks more and more like it’s been a life-long set-up that has now devolved into a lot of suffering.
Is it possible that an extreme episode of reduced brain blood flow may result in loss of memory for well practiced info such as one’s phone number or address? Similar to effects of a stroke but with no damage to blood vessels.
At worst I sometimes forgot my own name and couldn’t remember it even when I tried for five minutes before giving up.
After a crash I also lost basic knowledge on how to stand up from a chair when seated at a table or how to walk around my bed taking 90 degrees turns. I just had no clue on how to coordinate movements for both and had to actively relearn them.
So memory loss is definitely part of a bad spell of ME. Both temporary and more permanent with ability to relearn.
So far I believed it was due to the conditions the brain experiences when having ME can differ so much compared to the conditions when you learned the knowledge or skill that it fails to recall it. A bit like some people only can play darts when drunk but not when sober because they only play when drunk.
This has been described in POTS:
https://www.nytimes.com/2008/06/15/magazine/15diagnosis-t.html
Nice to hear good doctors find new types of OI. I often state I have some form of OI but no POTS.
Searching further on the topic I did find http://ether.stanford.edu/library/neuroanesthesia/SNACC%20Reading%20List%20articles/Oertel_efficacy%20of%20hyperventilation.pdf
With title: “Efficacy of hyperventilation, blood
pressure elevation, and metabolic suppression therapy in controlling intracranial pressure after head injury”
That tells a lot:
“With hyperventilation therapy, patients experienced a mean decrease in PaCO, from 35 ± 5 to 27 ± 5 mm Hg and in ICP from 20 ± II to 13 ± 8 mm Hg (p A whooping average of 35% drop in Intra Cranial Pressure should be a God-send gift for most patients with ME and or FM. Many recent blogs Cort posted deal with the strong association between too high ICP and ME/FM.
=> Reversed, if there were not an average drop in ICP by 35% or ICP going from 1x to 0.7x, not hyperventilating would increase ICP from 0.7x to 1x or an increase of 43% in ICP!
=> If indeed too high an ICP would be an important part in our diseases and higher ICP would correlate with more severe disease then increasing the already far too high ICP by another 43% by NOT hyperventilating would be an utterly debilitating and outright dangerous thing to do very likely to be far worse then the strong problems caused by poor blood flow to the brain.
=> Maybe we have here a main reason as to why we continuously hyperventilate and live with constant hypocapnia?
As to why hyperventilation would reduce ICP, this makes sense too.
Let us assume, with total fictive values as I don’t want to spend hours looking for actual ones now, the following 2 situations:
A) Normal ventilation.
* Blood from hart outlet has 100 units C02 per volume of blood.
* “Work”, thinking, in the brain consumes energy and creates 40 units CO2 per volume of blood in the brain
=> veins to the brain: 100 units of CO2 / volume
=> arteries from the brain: 100+40 = 140 units of C02 / volume
=> arteries are more dilated then veins making blood easier to flow back to hart.
B) Hyperventilation.
* Blood from hart outlet has 75 units C02 per volume of blood.
* “Work”, thinking, in the brain consumes energy and creates 40 units CO2 per volume of blood in the brain; granted if blood flow were reduced it may be a bit less but let me ignore this
=> veins to the brain: 75 units of CO2 / volume
=> arteries from the brain: 75+40 = 115 units of C02 / volume
=> arteries are more dilated then veins making blood easier to flow back to hart.
BUT: in the hyperventilation case ratios change. Numbers strongly suggest that in the hyperventilation the hypocapnia will hamper blood flow towards the brain more then it will hamper blood flow from the hart to the brain.
=> IF (needs some research/confirmation/numbercrunching) this were to be true, this would allow for a stronger reduction in blood inflow than in blood outflow. In other words: perfect conditions for draining pooling blood! And that in turn decreases ICP, blood getting “stale”, clotting of blood, I think inflammation too…
This also explains why at some of those very bad nights I have the following combination of observations:
* extremely unrestful sleep with loads of adrenaline and total extreme over the top nightmares
* breathing like a horse and still feeling I need to do more (aka “breathing my lungs out”)
* chest feeling like ran over by a truck in the morning, due to breathing so hard so long
The very high amounts of adrenaline increase breathing a lot (induces hypocapnia) and focus blood flow to the brain (partly compensating for the reduction in blood flow to the brain due to this very strong body-wide blood vessel constriction due to hypocapnia)
The “utterly insane” nightmares do two things IMO:
* Probably they pump up adrenaline to very high levels
* The nightmares are extremely vivid, full color, plenty of different types of action… and this seems to be a *very* strange thing for the brain to do as it should require plenty and plenty of energy to “produce” them. That is not something we would expect happens in a ME patient and certainly not in the moment of highest trouble.
BUT in the example above that very high amount of “work” done in the brain would increase units of CO2 produced above 40 to lets say 60, making in this example
=> veins to the brain: 75 units of CO2 / volume
=> arteries from the brain: 75+60 = 135 units of
IF the hypothesis is wright the totally weird, counterproductive and absurd would further improve reduction of blood pooling in the brain. The absurd would become the unlikely desired!
And it goes together with (part) of my “strange” nightly routine. One of the things that helps quite well is getting out of bed and just sit on a chair for 15 minutes. I thought since quite some time it was for “helping flow blood that pools in the brain back to the hart”. In the context of this and previous comment this totally makes sense.
Many people may think lying down improves blood flow to the brain due to gravity. It does: TO the brain, not away FROM the brain. That’s the reverse due to lack of help of gravity. As the night passes, pooling gets worse until it gets very problematic late at night / early morning.
Pre-constricting blood vessels body-wide by having low NO production should help too. It will restrict blood flow for sure, but it will improve the removal of blood versus the inflow of blood. It seems this is another mechanism not causing blood to pool but rather helping reducing blood pooling at the cost of poor body-wide blood flow. As such it resembles a lot an anti inflammatory measure produced by the body.
For those who might ask, I’ll write about my nightly ritual in the forum. I’m gradually building up to it in the “Me current improvement series”. Please have a little bit more patience if interested.
You are genial !That makes total sense to me. I will experiment sitting up in a chair for a bit when I awake early in the morning and my legs hurt and my adrenaline is throbbing .
Thank you. Heike
I’m mainly a good observer who has decided to look into some of those “totally impossible things” that happen over and over and over again. That’s likely unexplored territory where there is much to gain ;-).
Just moving a little bit the legs around when sitting helps too. Both legs and head seem to be zones of trouble in this sort of OI kinda thing. A few slow moves (while remaining sitting) up or forward go a long way.
It works both late midnight and early morning. I learned to do it most times when I wake up. In the beginning that meant I had barely any sleep left as it was chopped into pieces, but still I felt better. Now I wake far less often then before while having better health. Sometimes I’m a bit lax and just turn around and go and sleep again ;-). No need for perfection, just improvement. I skip a bit more in the morning as I often have a hard time to fall asleep again (in the morning, mid-late nights I just fall asleep asap). In the morning I just go to the toilet and back and fall often asleep again.
Please make observations while trying this out. Also take a look at symptoms as rapid or irregular hart beat, fast breathing, light headiness, chest pain in the morning… and please feel free to report any positives or negatives. I’d be very happy to learn more. When this topic would have died out, I’m also mail-able via Healthrising forum under the name dejurgen.
dejurgen : Read : The Downside of Upright Posture by Michael Flanagan, DC – a chiropractor with training in Neurology and physical anthropology – skull structure and how mammals, like whales and elephant seals, compensate for pressure changes. Yes, drainage from the brain is extremely important – and he discusses this. Sadly, Dr. Flanagan died in 2016.
Please I’d like to know more!
Correction:
=> Reversed, if there were not an average drop in ICP by 35% or ICP going from 1x to 0.65x, not hyperventilating would increase ICP from 0.65x to 1x or an increase of 54% in ICP!
On your “nocturnal moving around” hypothesis: throughout my gradual reversal of FM, I have been hyper-hydrating, involving drinking a lot of water and taking a lot of magnesium. I have tolerated higher frequency of urination as a side effect, as the benefits are clear. This includes getting up to urinate 2-3 times per night. I have long suspected that this enforced movement during the night, is also of beneficial effect.
I am convinced that “lack of movement” is when the worst fascial adhesions occur. The morning after some unusually high intensity exercise was always an ordeal, with stiffness, elevated pain, “muscle tissue tearing” sensations on movement, and extreme proneness to cramps on certain movements (eg flexing the ankles).
I hypothesize that the toxins produced by anaerobic exercise in particular, catalyse an increased adhesiveness of the fascia via the composition of the interstitial fluid, and adhesions occur during the next period of immobility.
On the other hand, I believe that “exercise avoiders” spiral down into debilitation from ever-greater encroachment of adhesions throughout their muscular system, even if they are not provoking this with anaerobic exertion. But deconditioning results in more and more mild forms of exertion becoming anaerobic, and the victim spirals ever-downwards in a vicious circle of effects. Even going shopping or taking a shower, followed by a return of inactivity, is deadly.
I have experienced massive benefit from increasing my aerobic threshold, as a by-product of avoiding anaerobic exertion but doing large amounts of low-intensity exercise. I can now do a lot while remaining aerobic (and not triggering relapses), that in the past would have required anaerobic exertion and would have triggered a relapse overnight.
I don’t say that getting up and moving around several times a night was “the” important self-help factor, only that it is one of many things that all help break out of a vicious circle for which there are many contributing factors. If one thinks in terms of interstitial adhesiveness, many things fall into place.
A lot of these new findings still don’t contradict my hypothesis about FM. I’ve beem saying for years that the stiffening, adhesions, and clumping of muscle fascia at crucial points around the body where there are complex intersections of both muscles and blood vessels, literally constricts blood flows in certain positions. The constrictions are “physical”, like slightly crushed copper pipes in a car’s engine coolant system.
This is not the same as vasoconstriction, which applies to the entire blood vessel. It is constrictions from external pressure at specific locations. Arguably, systemic vasoconstriction may increase systemic pressure to allow more flow through the externally squeezed points.
The other thing we know far too little about is what is going on in the “interstitial” spaces. The adhesiveness of fascia relates very much to the health of the interstitial fluids. The health benefits of Yoga and other movement routines is not “superstition”, it is straight-out medical biology, if you think of it in terms of mobilisation of interstitial fluids, preventing stagnation, local infection, and adhesiveness.
But there may be a lot more going on in “The Interstitium” than merely some kind of “inert” lubricant fluid movement – there may be actual vital biochemistry occurring that we know nothing about. Eastern medicine that refers to “energy flows” independent of blood vessels (and lymph vessels) may be vindicated yet.
I agree. I think the blood flow problem is system-wide. My painful muscles which sure feel like fascia problems to me – would agree as well.
If the small blood vessels are not working – then they must be impacting the fascia I would think.
If only a few good researchers would engage and could find a few patients with clear cases of these lumps, find them willing to do a not that pleasant small biopsy and look at it from all kinds off angles… There may be so much to learn. Would make a nice NHI project proposal…
I am a physiatrist (MD) that specializes in physical modalities for FM and ME/CFS. I was an ND prior. My most central modalities are Thai/Yoga therapy with myofascial techniques and teaching a host of controlled breathing techniques to raise or lower HR/BP. My clinical experience is that these work and work well.
Thanks Neilly,
Please welcome, everyone, the newest practitioner at the Bateman Horne Center. 🙂
According to Devin Starlanyl in her book on fascia pain, research has already identified a range of toxins that are present in what she and a network of researchers centred on Travell and Simons call “trigger points” (but she also calls them “nodules” of “contractured” fascia tissue, which is far more correct). Calling these “trigger points” immediately causes confusion with the common use of this term, which is not synonymous with lumps of stuck fascia tissue at all. This leads to otherwise very helpful scholarship being dismissed as a product of a confused mind, by “experts” vested in the mind / CNS / drugs racket.
Starlanyl cites J P Shah et al (2008),”Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points”
@Neilly Buckalew: thanks for doing so much needed work for FM/ME patients and thanks for taking interest in patients thoughts and concerns!
@Philip: I’m not only talking individual chemicals, but also “material properties”:
* Do fascia stick/glue to each other; if so, what is their “glueing” power and how does it compare to other sort of glue?
* Do fascia stick to other tissue? Same questions.
* What shape and size are individual cells once they are released from the strain of surrounding cells? How does it compare to cells of healthy people and cells of FM patients outside these lumps?
* Are these cells elongated? How does their volume compare to that of healthy cells (could indicate leak or overstretching by weak cell walls)? Are they bend (could indicate asymmetric change in material properties/composition/accumulation of toxins/asymmetric damage in cell wall)?
* Are they contracted e.g. shorter and wider e.g. more round shape?
I took out the latter as it demonstrates the importance of asking such questions. IF they were noticeably more round shaped for equal volume compared to healthy cells then a very identical process could be at work that makes RBC in ME patients round: strong oxidative stress damaging the cell wall.
Making the cells deform to a more round shape would achieve two goals when under high oxidative stress:
1) cell surface area would reduce, reducing exposure to oxidative stress external to the cell (ROS in the liquid the fascia are bathing in).
2) reduced cell surface area equals to a thicker cell wall (because the same mass used for the cell wall is spread over less surface area), better protecting the cell from ROS.
That would align with some of your observations:
1) If this effect took place on a fairly large scale it would shorten fascia, making muscle/fascia more tense and reducing range of motion.
2) As this mechanism would very likely be not homogeneous, it would cause a lot of local bending the fascia into irregular structures. Hard to predict how that would look, but knotty would be possible.
3) If I recall correct, fascia are more open type of structures. Having more round cells would reduces the amount of open space (filled with liquid) and make the fascia more dry as you mention.
Think about 1) and 3) like having all the iron beams in the Eifel tower replaced by beams half as long but twice the cross section area. Smaller tower, less open space between iron beams.
For 2) Think about the above but do not shorten all beams by a factor of two. Shrink each of them with an individual random factor between 1.9 and 2.1 (and change cross section area to maintain constant volume).
=> the result of doing the latter would be a very much shortened tower that is very bend in all kind of directions and has extremely strong local tension points making it nearly snap apart.
The above is just one of many possible outcomes of studying material properties IMO.
I have taken a class in blood vessel manipulation to relieve these kinks that you talk about. The most dramatic result for me came from a release of a neck/shoulder blood vessel restriction. One should be able to find practitioners in many metropolitan areas. Google should be able to help you out.
“The most dramatic result for me came from a release of a neck/shoulder blood vessel restriction.”
That was a really important one for me too.
Questions:
* Did it cause a remarkable and fairly rapid drop in pain levels?
* Where you hypothermia before and if so did that change with this treatment too?
I saw dr Novak for a number of years. Was 28 at the time went from great shape healthy to horribly ill. Had the low blood to the brain diagnosed by transcarnial Doppler. Pots tilt table. Turned out I had undiagnosed Lyme disease after many months of treatment and over a year of recovery time things have pretty much normalized.
Congratulations. So Lyme disease can cause this as well! Fascinating..I wonder what the bug is doing to cause the low blood flows to the brain? That is really interesting.I wonder if its neuroinflammation resulting in dilated blood vessels in the brain?
The treatment I guess was antibiotics?
I was one of the patients who Dr Stewart gave phenylephrine. It did “cure” my symtpoms for the day. Though things wore off. Clearly I creasing CBf helped me a lot.
Ha! Thanks for sharing that. I wonder how many people this applies to. Do you have POTS?
The oral version of phenylephrine works fine. It just has poor oral bioavailability.
My experience with Alpha-Adrenergic blockers Hytrin (terazosin). After rising and walking a short distance without any faintness I came to on the floor so weak could not move for several minutes,this happened three times, very scary. After research stopped the med no more problems.
wondering if that is why the “Meyers Cocktail” infusions work so well for a short while, not necessarily the micro-nutrients in them, but the extra fluid in the blood increasing blood volume and blood flow?
This hypothesis is a bit complicated for me to understand, but I’m going to try taking a phenylephrine tablet this morning and see if it seems to help my OI. Thanks so much, Cort, for this research review. Your work on our behalf is invaluable.
Sarah R, I’m heading to the drug store today!!! And hear, hear to Cort… three cheers ?
Thanks
Cognitive problems prevent me from completely understanding all of this info but I guess I don’t have to because I’m seeing Dr Chheda at Center for Complex Diseases. I have used 1-2 liters a day of IV saline for over a year. I can tell when I need it because of increase in cognitive problems, i.e. understanding people, finding words, the start of a headache, the need to lay down and completely remove myself from stimulation. I know some of this may not relate to OI but it’s interesting that I feel better after having saline. The Meyers Cocktail I tried 15 yrs ago lasted for about 1/2 hour. B12 shots and B supplements did nothing. But I just found out I have the MTHFR gene so that was the cause of the B vitamins not being metabolized, I think.
With the low blood volume found in ME/CFS and the effects that must have on getting proper blood flows to the brain, I think IV saline fits just fine into this discussion. IV saline allowed me, I think, to rapidly recover from an exercise test…
Dr, Cheney found low blood volume. This would cause not enough blood getting to the brain. But what causes low blood volume? Maybe eating extra salt helps??
As to the tilt table test – they may not be having the patient stand long enough. I passed out with no blood pressure at 28 minutes. I don’t think the docs know to test that long.
Lyme? Yes, but then why do some never recover on antibiotics? MAYBE some have an ongoing autoimmune response.
Yes, they may not be doing the tilt table test right. Low blood pressure often takes quite a while to show up.
The cause of low blood volume? That is a great and still unanswered question. I do remember hearing that if the blood vessels are unusually constricted blood volume will be down. (In this case it looks like the blood vessels are dilated though.)
It’s kind of amazing to me that no one had gone deeper into the causes of low blood volume.
My problems keep having me circle back to some kind of sleep disorder. But my home overnight pulse oximeter records a reasonable 90-99% O2 sat with a few apnea events yet I feel ill upon awakening. The one thing I’ve seen is many heart rate events where my heart rate sky rockets many times during the night with NO apnea or other visible or audible signs. I’ve used my home surveillance system to record audio and video and watched and listened during heart rate and apnea events. I see nothing to alert me.
I now see where I have no way of monitoring CO2 and hypocapnia while sleeping. It could be happening due hyperventilation or something else resulting in resulting in cerebral vasoconstriction. I asked multiple doctors why sleeping with supplemental O2 sometimes made a big difference but showed no “significant” O2 sat improvement. They said O2 sat said I was ok. One said my description sounded like a a shift in the oxygen–hemoglobin dissociation curve but that wasn’t possible. I investigated what might cause this including abnormal mitochondria and inadequate O2 tissue delivery at the cellular level.
Now I see it could actually be as simple as excess CO2 elimination and resulting effect on my brain blood O2 delivery.I have seen my Anion Gap varies wildly and is mostly high. Blood CO2 or bicarbonate levels (an anion) are adjusted by various mechanisms to offset cations.
Anion Gap = Sodium – (Chloride + Bicarbonate)
But the CO2 or Bicarbonate is mostly provided by respiration. So respiration issues that reduce CO2 can show up in the Anion Gap.
Has anyone seen a reasonable home CO2 monitor that would allow breathing levels to be monitoring during wake and sleep to look for hyperventilation or other causes that might be causing hypocapnia and its resulting effects?
I’m not familiar with measurements taken at home, but have you read any of the research on upper airway resistance syndrome? In particular, studies Stanford University and Dr. Steven Park describe this in detail and connect it to orthostatic intolerance. I’ve listened to a recent podcast Dr. Park produced proving that arousals are just as important as apnea events but aren’t routinely reported on standard sleep studies. This makes sense in my case. I have mild sleep apnea and feel faint on standing, etc. if my mandibular advancement device isn’t adjusted correctly. That tells me that my airway size definitely correlated with how I feel…definitely not cured but tremendously better.
Am I right that this links to the Hummingbird device? If I remember correctly, this increases blood flow. Would this help here?
I think it’s possible. If the Hummingbird can increase blood flows in the lower body it might be able to increase preload and thus blood flows to the brain. Low blood flows to the brain may be the key issue for all kinds of orthostatic intolerance..
Thank you – great article. Explains why I can think more clearly & quickly lying down & interestingly why I’ve noticed my thinking improves when I’ve had a cold and taken Sudafed (contains pseudo or phenylephidrine)
I wonder if vasodilation explains the alcohol intolerance. Or is there a known explanation for that?
Has anyone tried botox injections into the trapezious muscle to relax it and increase blood flow to the head and neck area?
That was supposed to be trapezius muscle.
I’m too wasted to follow everyone’s in depth comments right now. Do I understand correctly that there is no medical treatment available even if you are diagnosed with this new form OI? In other words, is it worth it to take my limited energy to go back to my OI cardiologist at this time?
Another great article Cort, well done!
Quick question regarding the link to a home test for postural hyperventilation:
Do we have a scientific citation validating the test we could show a doctor in the event one scores positive?
Here’s the test I’m speaking of:
“A Simple Hyperventilation Test
Take a breath and hold it: if you can only hold for your breath for 35 seconds or less you may be a chronically hyperventilator. Most people can hold their breath for 45 seconds or more.
A Hyperventilation Test When Standing
Stand up straight for 8 minutes.
If you start to feel ill stop and rest for a while.
Repeat the test but time breathe into a paper bag held across your nose and your mouth. If your symptoms appear when you are breathing into the bag you may be hyperventilating.”
Unfortunately I don’t know that there is. It’s been quite a while but if there was a citation I hope I would have put it in.
I have a lot of untangling and re-reading this to do— SO much of this spoke to my experience, not fitting with many traditional POTS symptoms, but definitely having parasympathetic misfiring. The sorts of things that are listed in the ‘POTS may also cause…’ lists that seem to include any symptom you can imagine.
I have a strange pattern when in a hard crash. There’s other signs, but I noticed (b/c was on IVIG and got a blood O2 monitor)—when I’m really sick, my blood O2 is 99 or 100. It’s normally 97. It’s not a huge difference, but it’s extremely consistent. I don’t know if I’m hyperventilating (I try very hard to control my breathing) or if the O2 in my blood is not being used properly, and then shows higher blood O2 levels. I’m not sure if the analogy fits, but I know I have testosterone that is being produced but other indicators show it’s not being used/taken up in my system.
Cort, are there any further investigations with phenylephrine?? The last study was in 2015
Not that I know of.
There was a question about fascia. To understand the complexities of fascia and health in a simple, straightforward manner I highly recommend David Lesondak and his book Fascia: What is it and Why it Matters. He expertly and wonderfully explains this area and its importance. I am writing another book with him now and a group of international experts that goes more into depth about fascia, a great unifyer of health, and covers a number of modalites/self healing techniques. I am back practicing in Idaho/Washington. One of my principal modalites is Thai yoga therapy with Chi Nei Tsang. Together these work all systems, fascia, immune/lymphatic, internal organs, and resets the nervous system into a parasympathetic state, in very short. Chi Nei Tsang is the ancient root of modern day pelvic physical therapy (see my colleagues presentation on BHC youtube), but is more intensive in addressing/resolving sympathetic overdrive, as it directly influences the brain vis a vis vagal afferents. I suspect given basic science evidence, the deep abdominal work of Chi Nei also positively impacts the microbiome as well. Clinically, I have seen 100% positive response using this modality that I have adpat to each patient’s needs. https://www.livingoak-integrated-medicine-and-rehabilitation.com
I have diagnosed POTS (tilt table) AND I have chronically low CO2 and trouble breathing when prone (sometimes when sitting as well). (My main symptoms are cognitive/neurological.)
Thoughts? Anybody else have both?
Does end-tidal CO2 testing go by any other names? I can’t find much on it except in terms of use in ICU.
“There’s also, less commonly, orthostatic hypotension (low blood pressure upon standing).”
Orthostatic hypotension is much more common than POTS, unless we are only considering young people rather than the whole population.