

We recommend that all ME/CFS and Fibromyalgia patients have a NASA 10-minute Lean Test to assess for orthostatic intolerance. Batetman Horne Center
The saga of the effort to introduce and validate the NASA Lean Test (NLT) for ME/CFS just seems so right in so many ways. First the Bateman Horne Center identified a test – from NASA no less – that can easily be used to identify orthostatic intolerance (symptoms when standing).
Then they enrolled a large number of patients, got researchers involved, validated the test, and in doing so, learned something new about ME/CFS in the process. It’s taken years to get through all this – but in the end, it provides something that’s really needed – an easy test to identify orthostatic intolerance (OI) and get doctors engaged in treating ME/CFS as a biological phenomena they can help with.

The NASA Lean Test, validated by the Bateman Horne Center, is easy – and requires just two simple instruments already found in doctors’ offices. (Image from the Bateman Horne Center)
Orthostatic intolerance refers to the inability to stand without symptoms. Although most of us are completely unaware of it, successful standing up requires an array of processes to work properly.
The minute you stand, gravity wants to force your blood downwards into your legs. In order to blunt that, the skeletal muscle pump constricts the blood vessels in your legs, increases pressure in the abdomen, causes a bit of swaying, decreases parasympathetic nervous system activity and activates the sympathetic nervous system.
The blood pressure at your arm momentarily drops as your blood starts to flow downwards, but then should bound back up as baroreceptors in the blood vessels tell your heart to beat faster. All this occurs automatically and below the level of consciousness.
When things go wrong with that system, orthostatic intolerance occurs and many different kinds exist. Postural orthostatic tachycardia syndrome (POTS) and its subsets (post-viral POTS, hyperadrenergic POTS, neuropathic POTS, hypo/hyperkinetic, exercise-induced POTS) appear to be the most common form of OI found in ME/CFS. Other forms of OI (orthostatic hypotension (OH), neurally mediated hypotension (neurogenic orthostatic hypotension) exist and, in this still rather new field, new forms of OI are still popping up.
Tilt tables have traditionally been used to assess OI but many medical practices don’t have access to them. The NASA Lean Test, on the other hand, can be done using the tools found in a doctor’s office. It requires only three things: an exam table, a pulse oximeter (placed on one hand), and a blood pressure cuff (placed on the opposite arm).
First, the person rests lying down for 10 minutes, then she/he stands up, and with her/his heels 6-8 inches from the wall, and shoulder blades touching it, stays there for ten minutes (or until it’s clear they have OI). Heart rate, blood pressure and symptoms are recorded. Just as the tilt table test does, the NLT removes the skeletal muscle pump action from the equation. You, your baroreceptors, your heart, and your autonomic nervous system are on your own.
J Transl Med. 2020 Aug 15;18(1):314. doi: 10.1186/s12967-020-02481-y.Hemodynamics during the 10-minute NASA Lean Test: evidence of circulatory decompensation in a subset of ME/CFS patients. Jihyun Lee 1, Suzanne D Vernon 2, Patricia Jeys 1, Weam Ali 1, Andrea Campos 1, Derya Unutmaz 3, Brayden Yellman 1, Lucinda Bateman 1
The large Lee-Bateman study (150 ME/CFS and 75 healthy controls) from the Bateman Horne Center consisted of ME/CFS patients who fulfilled the International Chronic Fatigue Syndrome Study Group research criteria (aka Fukuda), the Canadian Consensus Criteria (aka CCC), and the IOM clinical diagnostic criteria.
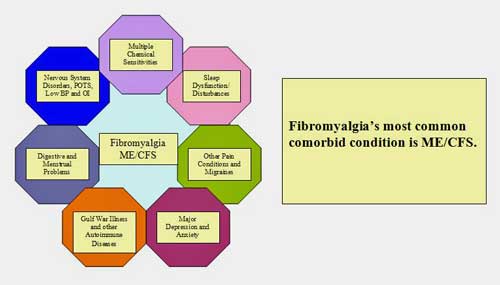
Many people don’t associated FM with orthostatic intolerance, but it is one of its comorbid conditions. Although the study was on ME/CFS, Dr. Bateman clearly states the NASA Lean Test should be used in both ME/CFS and FM. (Image from Wikimedia – https://commons.wikimedia.org/wiki/File:Fibromyalgia_and_comorbid_conditions.jpg)
All the participants benefitted from the Bateman Horne Center’s extremely thorough approach which included answering an astounding number of questionnaires (DePaul Symptom Questionnaire, Post-Exertional Fatigue Questionnaire, RAND-36, Fibromyalgia Impact Questionnaire-R, ACR 2010 Fibromyalgia Criteria Symptom Questionnaire, Pittsburgh Sleep Quality Index, Stanford Brief Activity Survey, Orthostatic Intolerance Daily Activity Scale, Orthostatic Intolerance Symptom Assessment, Brief Wellness Survey, Hours of Upright Activity, medical history and family history.
Besides heart rate and blood pressure, something called pulse pressure was measured as well. Pulse pressure is the difference between systolic and diastolic blood pressure. It represents the stroke volume – the volume of blood ejected by the heart when it beats.
Two kinds of orthostatic intolerance were assessed:
Orthostatic hypotension (OH) (lowered blood pressure upon standing) was defined as a decrease in systolic blood pressure (SBP) 20 mm Hg or more, or a decrease in diastolic blood pressure (DBP) of 10 mm Hg or more in the first 3 minutes.
Postural orthostatic tachycardia syndrome (POTS) was defined as a heart rate increase of >30 beats per minute (bpm) upon standing or a heart rate of greater than 120 bpm.
Results
Duration Matters – Less is not More
Time matters – this study validated the results of another tilt table study which indicated that the 1-3 minute orthostatic assessment typically carried out in doctors’ offices isn’t enough. Even a 2-5 minute tilt table test will miss a considerable set of POTS patients.
The Lee-Bateman study found that at least 5 minutes of the NASA lean test are necessary to pick up signs of orthostatic intolerance in most of the participants and a full ten minutes are needed to pick up more.
Interlude – the Plash study – More Can Be Tricky
The Gist
- Many people with ME/CFS or FM who have orthostatic intolerance (OI) ( their symptoms worsen upon standing) do not have access to the tilt table tests usually used to diagnose OI
- The Bateman Horne Center produced a study designed to assess the ability of a simple test called the 10-minute NASA Lean Test (NLT) which can easily be done in a doctor’s office.
- The NLT requires that patients stand with their backs to the wall with their heels 6-8 inches from the wall and shoulders touching the wall.
- The study found that about 40% of the ME/CFS patients meet the criteria for either postural orthostatic tachycardia syndrome (POTS) or orthostatic hypotension.
- It also found that the NLT test needs to be done for at least 5 minutes to get good results; 10 minutes is better.
- Because a significant percentage of healthy people who do not have orthostatic intolerance can test positive on the test, a diagnosis of OI requires that participants also experience symptoms while taking the test.
- The ME/CFS participants in the study experienced many more symptoms than the healthy controls. Their heart rate, blood pressure and pulse pressure readings were also significantly worse.
- Pulse pressure is an analog for stroke volume – the amount of the blood the heart emits when it beats. The low pulse pressure in the ME/CFS patients reflected reduced blood flows to the heart.
- David Systrom at Harvard found reduced blood flows to the heart (reduced preload) in his large study of people with exertion intolerance. He believes that microcirculatory issues that shunt blood into the interstitial spaces of the muscles may be robbing the heart of the blood it usually receives.
- People with shorter cases of ME/CFS (<4 years) were actually worse off. The authors believed that the systems longer duration patients may have created some compensatory mechanisms that may have helped.
- Diagnosing orthostatic intolerance in the doctor’s office could provide many people with ME/CFS and/or FM will treatments that help.
- The Bateman Horne Center believes everyone with ME/CFS or FM should have the NASA Lean Test done
Plash found out that while the 10-minute Tilt Table Test correctly identified 93% of the all POTS patients (high sensitivity), it also incorrectly identified 60% of the healthy controls as having POTS (!) (low specificity). After 30 minutes of the tilt table test, things were considerably worse: 80% of the healthy controls were incorrectly identified as having POTS.
The Lee/Bateman study found the same. At the end of ten minutes, 33% of healthy controls meet the criteria for POTS (increase of <30 bpm). (Forty percent of the people with ME/CFS did.)
The issue arises because even the heart rates of healthy people tend to increase over time when they are tilted. Plash suggested that at the 10 minute mark, the criteria for having POTS should be increased from 30 bpm to 37 bpm, and at the 30 minute mark, to 47 bpm.
Note that even using this stiffened criteria, the tests were not completely accurate; i.e. they still falsely identified from 20-27% of healthy controls as having POTS. This isn’t much of an issue for people with ME/CFS/FM with orthostatic intolerance issues (symptoms increase upon standing or after standing for awhile, but it’s interesting that some healthy people – and probably not a few – have POTS-like increased heart rates upon standing. For some reason, they don’t suffer from POTS.
The issue also makes clear that increased heart rates by themselves don’t necessarily produce POTS. It’s a multidimensional illness – some aspects of which we clearly don’t know much about.
Plash concluded that POTS should only be identified in people with symptoms of orthostatic intolerance and high heart rates on a TILT or standing test like the NASA Lean Test (NLT). The Bateman Horne Center concludes the same – high heart rates during the NLT are only diagnostic for POTS if they are accompanied by symptoms as well.
Symptoms, however, were not hard to find in the chronic fatigue syndrome (ME/CFS) group. The test provoked far more symptoms in the people with ME/CFS patients – even in those without POTS (see below) – than it did in the healthy controls.
“Pathologic” Drops in Pulse Pressure
The ME/CFS group also has worse cardiovascular scores. While both groups’ heart rates increased over time, the heart rates of the ME/CFS group started out higher (that high baseline heart rate issue) and went up faster. In fact, every measured test result (blood pressure/ heart rate/ pulse pressure) was worse in the ME/CFS patients than the healthy control group.
Higher heart rates (both resting and standing) and “pathologic” drops in pulse pressure particularly distinguished the ME/CFS patients from the healthy controls.
The “striking finding” of the very abnormally narrowed pulse pressure in shorter duration ME/CFS patients (<4 years) appears to have reflected a reduced stroke volume; i.e. reduced blood outflows from the heart. That is usually the result of a heart problem, but studies suggest the heart in ME/CFS is generally fine. Instead, the authors asserted that narrowed pulse pressure was almost certainly caused by reduced blood inflows to the heart.
That ties in nicely with what Systrom found (reduced preload) in his invasive exercise study. Systrom believes several things may be in play, including microcirculatory problems which are reducing blood flows to the venous system (the left to right shunt) causing less blood to be available to the heart.
Newbies Are the Worst Off
Interestingly, the more recently a person came down with ME/CFS, the worse off they were. The relative newbies – those who have been ill for less than 4 years – had the worst drops in pulse pressure, followed by those who had had ME/CFS for over ten years.
Why would people newer to ME/CFS have worse problems than those who had it longer? Perhaps because some sort of compensatory approach over time been developed. The autonomic nervous system can be trained and it can apparently adapt to some extent. My symptoms were certainly worse in the beginning.
Orthostatic Intolerance Without POTS or Orthostatic Hypotension
That study also found that even ME/CFS patients who didn’t meet the criteria for either POTS or orthostatic hypotension still experienced significantly more symptoms during the NLT than did the healthy controls. Somehow, they too were getting whacked by having to lean up against a wall for ten minutes. That finding reminds us that the field of orthostatic intolerance is relatively new, surprises are in store, and that POTS or OH isn’t everything.
The field is also growing and the authors were able to point quickly to a 2020 study by Van Campen and Visser, which found that even ME/CFS patients without POTS or orthostatic hypotension still experienced reduced blood flows to the brain during a tilt test.
I may have experienced something like this during a twin study about 15 years ago. Both my twin and I “passed” the tilt table test, but I was miserable throughout and remained symptomatic for some time afterwards. He, on the other hand, experienced no symptoms at all.
The Visser study followed a 2018 study by Peter Novak, who also uncovered a group of patients without POTS or any other sign of OI, but nevertheless had reduced blood flows to the brain. Novak uncovered this group after he kept getting “POTS” patients who didn’t end up having POTS. What they did have were low CO2 levels. Novak called this new form of orthostatic intolerance hypocapnic cerebral hypoperfusion.
Novak suggested a number of possible causes (baroreceptor problems, metabolic acidosis, orthostatic ventilation-perfusion mismatch, problems with the respiratory centers in the brain) and was planning to dig deeper. Since this is probably not a small group, and since it’s clear that it’s abundant in ME/CFS, further investigations into this group are going to be fascinating.
If you’ve been disappointed when your non-POTS diagnosis failed to capture your brain fog, standing problems, etc. – be disappointed no more. There are clearly other ways to mess up your brain when you stand than by having a fast heart rate or a balky blood pressure adjustment system.
Treatment
While the study didn’t provide treatment recommendations, many treatment options exist. That’s good news for you and your doctor. On the one hand, seeing your doctor may actually help you to get better (woo-woo). On the other, your doctors get to do what they got into their profession to do – help you. Maybe they’ll even get more interested in ME/CFS or FM.
The symptoms associated with orthostatic intolerance closely resemble those found in ME/CFS and FM, and include lightheadedness (occasionally with fainting), difficulty thinking and concentrating (brain fog), fatigue, intolerance of exercise, headache, blurry vision, palpitations, tremor and nausea.
From doing things like increasing salt intake to increasing blood volume, to wearing compression stockings, to drugs, to recumbent exercises (for those who can handle them), many options are available for people with OI.
- Check out Health Rising’s Resource Center for Orthostatic Intolerance to learn more about diagnosis and treatment options.
Check out some videos from the Bateman Horne Center on how to diagnose and treat orthostatic intolerance:
Conclusions
The main finding was that many cases of orthostatic intolerance can now be diagnosed in a doctor’s office using the simple tools embedded in the NASA Lean Test. All a doctor needs to do is assess symptoms, heart rate and blood pressure for ten minutes. Orthostatic intolerance is diagnosed when the following guidelines are met – in the presence of symptoms:
- Orthostatic hypotension (OH) – (lowered blood pressure upon standing) – a decrease in systolic blood pressure (SBP) 20 mm Hg or more, or a decrease in diastolic blood pressure (DBP) of 10 mm Hg or more in the first 3 minutes.
- Postural orthostatic tachycardia syndrome (POTS) -a heart rate increase of >30 beats per minute (bpm) upon standing or a heart rate of greater than 120 bpm.
Health Rising has a ‘how to’ for the NASA Lean Test from Dr. Lucinda Bateman here. Note that the test is most revealing if the patient:
- Limits water/fluid intake to 1000 mL for 24 hours before the test
- Limits sodium intake for 48 hours before the test
- Does not wear compression socks or compression clothing on the day of the test
- Withholds medications, supplements, or substances that might affect blood pressure or heart rate, with timing based on the drug half-life and patient safety. (See the post for the list.)
The study also revealed that tests for OI must be at least five minutes long, that orthostatic intolerance can only be diagnosed in people with symptoms of it, that some healthy people have high POTS-like heart rates, that the orthostatic intolerance in people who are relatively new to ME/CFS (<4 yrs) is worse, and it suggested that Systrom’s findings of reduced preload or blood flows to the heart are accurate. That suggests problems with the microcirculation are losing blood somewhere along the the way.
The study found that about 40% of the ME/CFS patients tested positive for orthostatic intolerance, but a recent Visser study found that over 80% of ME/CFS patients who did not meet the criteria for orthostatic intolerance still had reduced blood flows to the brain. Not testing positive for POTS or orthostatic hypotension does not mean you don’t have orthostatic intolerance. You could, for instance, have the new form of OI uncovered by Novak – hypocapnic cerebral hypoperfusion. There is clearly more learn about OI.
- Coming up – a cheap and effective replacement for saline?


 Health Rising’s Quickie Summer Donation Drive is On!
Health Rising’s Quickie Summer Donation Drive is On!



Question
i am wondering if there is any link
between heat rate and either systolic or diastolic blood pressure?
( where, for example,
the beats per minute
is the same number
as systolic or diastolic blood pressure?)
Systolic blood pressure refers to the force of the blood against the arterial walls when the heart beats. After that contraction or beat is done the blood pressure falls – that is the diastolic heart pressure.
Heart rate simply refers to how fast the heart beats.
Hi, I am living in the Netherlands patient to Erasmus MC hospital . My bloodpressure is also fluctuaties. We called it as bovendruk en onderdruk. I am hoping my reaction can be translate to English. Described as 180 bovendruk en 90 onderdruk. Als ik uit bed kom gaat mijn hart te very fast , en als ik de bloeddruk meet is het 140 bovendruk en maar 68 onderdruk. De pols wisselt voortdurend van soms wel 58 slagen tot 130 slagen per minuut. Erg moe en vreselijk hoofdpijn, pijn op borst en benauwd, vervelend gevoel op borst, slapeloosheid, vreselijk veel pijnen ook neurologische en neuropathische.Ik heb Sjogren primair, fibromyalgie, Forestier also called Dish, mitralisklepinsuffiscientie, distale renale tubulaire acidose. 2x pericarditis, gevoelstoornissen huid, polyartrose polyneuropathie. Brainfog!!! Ben heel blij Sjogren’s Advocate en deze site gevonden te hebben. Dankbaar. Ik weet nu meer dan ooit . Alleen de artsen nog en mijn familie. Wat je niet ziet heb je niet. Warmte en koude intolerantie. Etc. Hartelijke groeten en veel sterkte voor iedereen.
Alma Siereveld
thank you for describing your symptoms and your kind words, as for everyone, i wish a cure for you too. warm regards to everyone who replied.
Thank you Sunie, my English is not so good but I hope you have understand something.
I would experience lightheadedness, high pulse rate, nausea and I think drops in blood pressure but not all of the time. I don’t think I’d be categorised as having POTS though.
If this occurs, I can feel horrible for hours. It’s one of the symptoms I fear the most – feeling like I’m just about to faint is very unnerving.
My blood pressure fluctuates now. Before becoming unwell, I never had high blood pressure apart from when I was pregnant. It can go very high or a bit low and it can drop quite quickly. It’s settled a bit at the moment and I’m not entirely sure why. I suspect the nervous system is involved.
To stop myself from feeling faint, I eat dark chocolate and I suppose that brings my blood pressure up. It’s something I am aware of throughout the day. But I know when I’m okay and when I’m not.
I also think brain glucose has something to do with my symptoms. I am very limited in the carbohydrates I can tolerate, as I seem to have a difficulty with fructose, all the grains, milk etc etc
I have improved recently because I was eating some chocolate chip cookies and sweeter chocolate – which then brings all sorts of other problems. However the near fainting episodes have stopped. I generally don’t have a detectable issue with my blood sugar as such, I think the problem is in my brain, which is tricky to access. I’ve been checked for diabetes, which comes back negative and I have my own blood sugar monitor – given to me by my doctor – I think to give me something to do and to stop bothering them!
Okay last thing – chocolate and chocolate chip cookies raise dopamine levels. So, what if the body/brain is purposefully keeping me at a lowers functioning state ie Naviaux’s Dauer theory? And that I’m attempting to over ride this program.
Tracey Anne,
I am always grateful to read your experience, for i identify with so many difficulties and anecdotal helps. I find chocolate helps, but wonder ad you do if it is from a boost in dopamine. Best wishes,
ad always, sunie
Hi Sunie 🙂
Yes, the chocolate chip cookies are still my standby. I don’t know why they work but they still do. I have some at the moment, in the glove compartment of my car. And milk chocolate works too but it makes me feel sick, if I eat it repeatedly.
I certainly hope the cure for CFS turns out to be chocolate chip cookies. Although, if that is found to be the case, I’m sure the chips will quickly be listed as a Schedule III substance and we’ll all be begging our physicians for an Rx (despite the hundred-fold increase in price).
While waiting for the relevant studies to be conducted by Nestle, and Phase 1-3 trials conducted by their partners at Pfizer, I have questions about your broader approach.
You say you have “difficulty with fructose, all the grains, milk etc”, but chocolate chip cookies are traditionally made with wheat (a grain) flour, and sugar (i.e., sucrose, which is broken down in the gut by sucrase into equal parts glucose and fructose), and butter (which is made from whole milk). In spite of all that, you claim you’ve improved BECAUSE you’ve been eating chocolate chip cookies and sweeter chocolate.
You say your problem is with your brain. (Bingo! I have my own!) Then you say the problem is your “brain glucose” – is that a thing? Isn’t the glucose in the brain the same as glucose in the blood? You say you’re checking your blood glucose. Have you found some connection?
In another comment, you say that chocolate chip cookies increase the dopamine in your brain. How do you know that to be true? How do you measure that? And, if it does, what does that even mean, relative to brain (or other) performance?
In yet another comment, you say you felt very peculiar – and blame it on your blood pressure being “off kilter”. Did you measure it? Do you track that variable vs your mental or energetic states, a dozen or more times a day, in order to establish a connection?
My blood pressure easily varies 20mmHg in a five- or ten-minute measuring session. Is that due to my ANS? Is it due to measuring error? I can’t claim to know, so I don’t.
My cognition varies dramatically from day to day, and from hour to hour (along with my energy and my pain), but – despite eating a very limited, relatively “healthy” diet – I’ve not been able to establish the powerful correlations you have, despite looking for 35 years.
My point: it doesn’t do you, or anyone else, any good to come to conclusions about cause and effect unless you are doing the work that is necessary to establish that relationship. Or, [there was a salient rephrasing of this point in my head 30 seconds ago that is now gone to the cerebral graveyard in my head]. So, I’m off to bake some cookies. I hope it works!
Feral Boy, I don’t know the answers – in the absence of any help, I’m trying my best – do you have any helpful suggestions?
Usually people on Health Rising are supportive of each other. You remind of my doctor, family, etc etc who question my illness, my experience, my sanity, undermine my intelligence and so on. I’m quite used to it… I’m just not sure what you’re trying to achieve?
I was quite upset to read what you wrote but years of surviving being very, very unwell, being a lone parent, with few resources, facing derision, oppression, isolation and so on, has thankfully made me really tough and resilient.
I feel upset but if you’re on this site, you’re probably very unwell too – I actually don’t want to spread the negativity further and so I send you my best wishes instead.
Tracey
I wonder if you have a form of orthostatic hypotension – which is a sudden drop in blood pressure. It sounds, though, like your system is dysregulated – trying to find a balance and sometimes failing. The baroreceptors in your heart and neck assess blood pressure. One idea about all this is that something is the matter with the baroreceptors – they’re either not assessing pressure in the arteries correctly or the signal they send to the brain is getting messed up.
Dysregulated sounds right and yes, I would seem to have sudden drops on blood pressure. One day when I was aware that my blood pressure and pulse rate were all over the place, I sat down and just kept taking my blood pressure which was I think up at around 137 systolic and then it went down a bit and then suddenly dropped to 110.
Last month I was having a socially distanced cup of tea, outside, over at the neighbours and I felt very peculiar – I know my blood pressure was off kilter – I was nauseous and really uncomfortably horrible – I went home but continued to feel unwell for hours.
The choc and choc chip cookies put my blood pressure up, pulse rate up, give me energy and somehow seem to over ride the imbalance or force a new normal or whatever. I don’t know. Having a sleep in the afternoon, seems to reset something and I’m fine first thing in the morning.
I’m so used to it now, it’s just something I have to deal with throughout the day and I CAN feel absolutely fine – so sometimes I feel a bit of a fraud and think – you see you’re okay. I’m just very unstable and I can’t just take things for granted – which is very difficult to explain to others.
I often feel as though I really shouldn’t be meddling with these systems – I’m out of my depth and choc chip cookies are not a very advanced intervention.
I did try some caffeine tablets fairly recently – that went very badly wrong. One tablet is 50mg of caffeine. I took one and seemed okay and then took another one later in the day and again seemed fine. However that evening my blood pressure shot up to over 170 systolic. I thought I’d better go and lie down but I was so aware of my heart beating, it just made me worse. So instead I went for a slow walk with my dog. I returned to normal eventually…
Tracey Anne, you may want to do the Nasa Lean test at home. You may be surprised what you can learn from it. It’s not just the numbers – it’s recreating the symptoms. You may be able to learn which of your symptoms may be ascribed to autonomic dysfunction.
(a lot of your symptoms fall in line with POTS… feeling better after laying down = horizontal. To be fair, differential diagnosis CFS leaks….)
And just a thought: chocolate/chocolate chip cookies = potassium? magnesium? does it do something to calcium? hmmm
Thanks Meirav, very interesting and your comments below. If I could sort this issue, I wouldn’t be too bad.
Bateman Horne’s great. I’m a bit overwhelmed by all their information. I’ve joined a couple of their support groups via zoom. Have computer + internet – will travel!
Sounds like you may need your cortisol levels checked? Symptoms you describe are how I feel when my cortisol is low. I have adrenal insufficiency/Addison’s
Do you mean me Melissa? No I haven’t had my cortisol levels checked and I have wondered whether they could be low, or lower than I need them to be.
I will be printing this article and sending to local health care professionals. All GP’s, Pediatricians and OBGYN offices should do a better job of looking at these issues. Additionally, the Cardiologists really should start looking for hypotension. You can help the situation by mailing information to doctors offices.
“Pulse pressure is the difference between systolic and diastolic blood pressure. It represents the stroke volume – the volume of blood ejected by the heart when it beats.”
I can’t imagine that’s correct. My pulse pressure is higher than normal but my stroke volume is much lower than normal, according to Dr. Cheney.
“we know the heart in ME/CFS is generally fine.”
If by that you mean systolic function (ejection fraction) is fine, or that most cardiologists think that ME/CFS patients’ hearts are fine, OK. But with Peckerman’s help, Dr. Cheney identified diastolic dysfunction as well as PFO’s in his patients.
I agree that Dr. Cheney’s finding does not comport with these results. We could be missing something though.
Here’s the definition from Wikipedia
https://en.wikipedia.org/wiki/Pulse_pressure
“Pulse pressure is the difference between systolic and diastolic blood pressure. It is measured in millimeters of mercury (mmHg). It represents the force that the heart generates each time it contracts. Resting blood pressure is normally approximately 120/80 mmHg, which yields a pulse pressure of approximately 40 mmHg.”
“The systemic pulse pressure is approximately proportional to stroke volume, or the amount of blood ejected from the left ventricle during systole (pump action) and inversely proportional to the compliance (similar to Elasticity) of the aorta.[4]”
It is not a perfect surrogate, though.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4054969/
“Arterial pulse pressure has been widely used as surrogate of stroke volume, for example, in the guidance of fluid therapy. However, recent experimental investigations suggest that arterial pulse pressure is not linearly proportional to stroke volume.”
The authors stated that reduced pulse pressure is usually due to restrictive pericarditis, an outflow obstruction (aortic or pulmonary stenosis), pump failure from a diseased heart, or shock (anaphylactic, septic, cardiogenic) – none of which applied to ME/CFS. My guess is that diastolic dysfunction would fit into the pump failure category. However, I wonder if the DD Cheney found could be due to less blood flowing into the heart.
Unfortunately Dr. Cheney never published his results in a scientific journal. Montoya did what appeared to be a pretty thorough assessment of the structural aspects of the heart here – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5807550/ – and found no differences.
Some studies have found small hearts but I believe they may be due to deconditioning or reduced blood flows to the heart.
Cheney’s diastolic dysfunction was never really embraced by the ME/CFS researchers. I don’t know why. As I remember he thought it was more a energetic problem than damage to heart. If that’s true he could still be correct.
If it had been damage to the heart my guess is that it should have worsened over time and lead to heart failure -which it obviously didn’t.
I haven’t followed Chaney’s work, but perhaps I can shed some light on this slim fraction of the conversation. The heart’s left ventricle contracts, creating pressure; flow into the atrium is blocked off by an internal valve, so that pressure is directed only to the aorta and into general circulation. The difference in pressure between the ventricle (high) and the body (not so high) causes blood to flow. The back pressure from bodily circulation is not constant – it’s going to depend on the ventricle’s pressure, and the ever-changing geometry of the capillary bed, and – I’m sure – other stuff I’ve never heard of. The pressure from heart contraction is dissipated into the blood flow, and eventually reaches equilibrium with the venous system (i.e., on the other side of the capillary bed resistance); at that point – diastolic pressure – flow more-or-less stops.
It’s true that there is a relationship between pulse pressure and stroke volume, but they’re obviously not “equal” – they use different units [force/area] vs [volume]. The wiki article, or a comment, said it is proportional, but that is also obviously not true – there are far too many factors – although it might approach that relationship under limited conditions.
For a given person, with a given capillary bed resistance quotient, in a typical range of functional pressures, the relationship would be very roughly proportional (though it would still differ due to aortal and arterial elasticities, etc).
It’s also true that a given pulse pressure would result in radically different stroke volumes, due to the varying back pressure that results from different physiological conditions in a single patient, or in the different circulatory geometries/states of two different patients.
Re: the comment of “Tim”, if you have a very high capillary back pressure, as has been hypothesized by Les Simpson (due to RBC deformity, circa 1990s) or Ron Davis at Stanford (due to constricted capillary geometry, 2019), or me (since about 1990), then a high pressure pulse may still result in a low stroke volume – just as a garden hose bib will release a low flow of water if the valve is almost shut (creating high back pressure).
Orthostatic intolerance is more broadly the idea that people can have difficulty standing or sitting. For many people with ME/CFS there may not be a change in blood pressure or heart rate. Rather, we find that lying down for a half hour or more can make a significant improvement. Often I find the brain fog disappears after lying down. I can have a very active mind, start composing emails in my head, only to go sit at a computer and have a complete blank.
The heart issues affect the delivery of oxygen to the brain, as we’ve seen in a number of studies.
GP’s and cardiologists tend to discount reports of orthostatic intolerance that fail to fit the heart rate or blood pressure metrics.
“GP’s and cardiologists tend to discount reports of orthostatic intolerance that fail to fit the heart rate or blood pressure metrics.”
Exactly – once again we’re coming up against traditional norms. That Visser and the Novak papers are fascinating in that they suggest that many of us who do not have HR/BP problems still have OI.
Yes, my symptoms were not investigated for years. Turns out I have OCHOS, which can only be detected with a transcranial Doppler ultrasound.
https://pubmed.ncbi.nlm.nih.gov/26909037/
(It turns out I don’t have CFS, but many people with CFS coukd also have OCHOS.)
As many of you know, POTS and NMH are very common in Ehlers-Danlos Syndrome–as is fatigue.
In my quest for attempting to increase my energy, I finally will be getting a Stanford appointment to look at my super labile HR and BP–with an actual Tilt Table Test! Although I don’t have much pre-syncope, I am a fidgeter and find it very difficult to remain standing for long periods of time. My PCP’s are always advising the usual; drink more fluids, take electrolytes, especially salt, wear compression garments etc.–all to no avail.
Because dysautonomia is so common with EDS and so difficult to regulate, there are a small number of doctors who are fussing about with using various medications to try to control it. The latest EDS book ‘Disjointed’ has several chapters with lists of these drugs. Also Dr. Peter Rowe and Dr. Alan Pocinki are two medicos who are very involved with the junction of ME/CFS, autonomic dysfunction and EDS and one can glean a lot of information from their research and lectures.
I’ll probably report back after my experience. I’m always searching…
As far as my ‘experiments’ with thyroid medication, seems as if I might have a T4 to T3 conversion problem which is likely genetic. I am getting some noticeable improvement but still have a ways to go…
Once again, thank you for these blogs, Cort!
That they made the instructions on how to do this test at home available for everyone – has been a life-saver for me:
1. I learned to recognize the mysterious symptoms – in a very specific order of appearance – as POTS. I’ve had them from a young age, and got worse the past 7 years. I had been going to doctors to investigate hypoglycemia and insulin resistance (in the absence of high plasma glucose)
2. I learned that as my pulse rate narrows, that’s when I start to feel that I’m about to pass out (I couldn’t do the full 10 minutes, it got down to 18 mmHg)and that was enough for me)
3. Because I know what my autonomic system is doing thanks to the test, I was able to advocate to get the correct diagnosis. The POTS specialist in my country of residence is one with the strong opinion that the tilt test shows what it needs to in the first – he says three minutes, but with me he gave up at one… Most doctors and health advocates will believe a fellow doctor before a patient.. you guys know well how that goes. It’s been the piece of paper with my lean test results that made the difference.
4. THIS is priceless to me. I email the Bateman Center thanking them every few months, when the piece of paper has once again helped me in some way in front of the medical establishment.
One thing they fail to mention is orthostatic hypertension.
Pulse pressure is also all over the place – can be quite wide at times. It just seems like my heart is constantly compensating and adjusting its variables, attempting homoeostasis.
I’ve developed labile blood pressure as my POTS has gotten worse in the past decade (and even orthostatic bradychardia at times). As such, treatment is tricky, the experts say. They still haven’t settle on one proven way.
I have seen interesting results by supplementing 1-Carbon metabolism, guided by my blood test results.
One nutraceutical normalizes my blood pressure AND heart rate. I can see how long a dose lasts because as I take measurements, I can see the instability returning.
Another nutraceutical affects only the pulse pressure. What this means is that I still have the big orthostatic jumps in both heat rate and pressure BUT no symptoms. No symptoms also means no nausea, no throwing up, no excessive drinking and flushing of water (so maybe this will make a dent on my sodium potassium levels, which are low).
It’s still too early to know the sustained effect.
I’m still tinkering.
Meirav, would you be willing to share what is in neutraceuticals and how using them?
Could someone also explain how to determine if pulse rate is narrowing?
Thank you in advance.
I think you would take your blood pressure and determine the difference between the high (systolic) reading and the low (diastolic) blood pressure.
A pulse pressure is considered low when it’s less than 40 mm Hg. A high PP is greater than 60.
https://www.healthline.com/health/pulse-pressure#low-pulse-pressure
sunie, I’m guessing Meirav mistyped “pressure pulse narrows” – meaning a decrease in the difference btwn systolic and diastolic pressures – as “pulse rate narrows”.
Damn it: “pulse pressure”, not “pressure pulse”
I learned about pulse rate from the test. Calculated as Cort wrote. You can follow the instructions on how to do it on their website.
https://batemanhornecenter.org/wp-content/uploads/2016/09/NASA-Lean-Test-Instructions.pdf
You do need to have supplies for oral dehydration at hand for after the test, if you are one who is affected from doing it. They do have a list but I can’t upload it here…
(Salt doesn’t do it for me; it makes my nerve bonkers)
Had I not known about pulse pressure, I would have looked at my blood pressure and heart rate measurements while on the nutraceutical and assumed it was not doing anything to my cardiovascular/autonomic system (and yet ameliorating the symptoms).
Oral ‘rehydration’, that would be.
HI Sunie – I’m a little reluctant to share which nutrients (supplements) I am using as it is based on my blood tests, and spending time learning a little about the biochemistry of certain amino acids. The dose makes the poison too. I sometimes end up causing certain symptoms to get worse, and I can take responsibility that I’m a walking experiment. Responsibilities for others’ health… that would mortify me if someone else were to get sicker.
What works for me may not work for you – it’s quite a personalized approach. I’m still tinkering with things myself.
I can recommend that you get yourself tested for all the vitamin Bs, and any nutrient you can, and plasma amino acids – urine if it’s available to you. There are ways to do it through your health insurance.
It is my thinking that sometimes it is not necessariy numbers but relationships between substances that is important.
If it is possible for you to work with a doctor (functional) that can help figure things out with you, that would be ideal.
I think a safe place to start is anti-oxidants. We may need copious amounts of them. I’m a fan of vitamin C. in sublingual or liquid form may be best. Bilberries and other anthocyanins if you like your sources more natural. Vitamin E is also on the list (haven’t tried it yet). Glutathione, CoQ10 – I don’t why, I’m not keen on them…
Cacao also – there is a specific form (less refined, the purest kind?) there are studies in to it being high in anti-oxidants. Think aztec cacao. Mars in the States makes it, from what I remember. I
Thanks Cort for summerizing this research. Thanks to all of you. How do you measure at home the pulse. They are showing an equipment on the finger. Do you messure the pulse and the pulse pressure? are these 2 different things?
Ruti, click on the link in Cort’s article for the full study. Access is free.
Pulse = heart rate (HR), measured in beats per minute (bpm). If you measure BP with an electronic cuff it usually also reads HR. You can also measure HR using a finger cuff, or by counting the beats in a unit of time and calculating for bpm.
Definitions from the study:
Systolic BP (SBP), diastolic BP (DBP) and HR were used as raw values recorded during the 10-minute NLT.
Pulse pressure (PP) and narrowed pulse pressure (NPP) were calculated according to the consensus equation: PP = SBP- DBP and NPP = PP/SBP.
PP is considered abnormally narrow if it is less than 25% of SBP [12].
For assessing OI manifestations, changes in HR and BP during the 10-minute NLT were classified as follows.
OH was defined as a decrease in SBP of 20 mm Hg or more, or a decrease in DBP of 10 mm Hg or more in the first 3 min standing compared to resting supine values.
POTS was defined as an increase of HR greater than 30 bpm or a HR of greater than 120 bpm, based on the average of the last three minutes standing. (e.g., if the standing portion of the test was terminated at 6 min, we calculated the mean of the data recorded during the 3rd, 4th and 5th minutes).
Feral Boy, Meirva, Cort (and for your continued dedication/ blogs)
thanks for explanations—especially the longer ones
also helps those especially who have limited data
I thought that you needed a break of about 10 minutes between taking blood pressure or the results become altered simply by the process? Perhaps that only happened with old monitors like mine? However, it means I can’t try this at home
The test requires that you lie down for 10 minutes first and then stand up and do the test.
Don’t you have to take multiple readings of blood pressure, though?
Diane (Disne) maybe discuss with your health care provider how to do test at home— or if anyone you know might have a serial bp / heart rate machine that you could use?
?would the following be safe and give you some data?
taking bp at start of laying down, then at ten mins laying down, then stay laying down another ten mins and see if blood pressure staying same.
if bp is staying same,
if you can do it safely, try standing (lean) for ten mins— if you can have someone there to monitor and write your symptoms down as you feel them,
and have assistant turn on bp machine and record reading at ten mins
if still okay and can continue safely enough,
have assistant turn on bp machine after another ten mins and record reading
Hi Diane –
You can follow the instructions here. It includes a log sheet for taking down measurements: https://batemanhornecenter.org/wp-content/uploads/2016/09/NASA-Lean-Test-Instructions.pdf
You need someone to take the readings and write them down. You are not to move and speak only to communicate symptoms as you experience them for the other person to write them down. You can use cuff or wrist sleeve bp machine.
You lay down until your BP and heart rate are normal. 10 minutes or more if you need them. Then you stand up against the wall, and take readings every minute until minute 10. Unless you feel so sick or are about to pass out and need to stop it before. Read the instructions, because there are things you should do from the day before, and when it is best to do, etc.
Also, make sure you have oral rehydration supplies at hand, in case you need them.
Things like electrolytes, hydrations salts, IV saline solution, V8, broth per their list (gatorade?). They “recommend salt, fluid loading which can include rehydration liquids. Other interventions include compression clothing, elevating legs and rest.”
(Salt makes my nerves go bonkers, so…)
The beauty of this is that you can do it at home.
Some doctors will say that high readings are due to white coat syndrome.
Doing it at home does away with this.
No more excuses.
These instructions have a space for recording BP every minute.https://batemanhornecenter.org/wp-content/uploads/2016/09/NASA-Lean-Test-Instructions-1.pdf
To Anyone of you — why does this make some of us have so very much trouble with the heat? Both indoor and outdoor, both summer and winter
Also, Cort, I looked up your homebrew recipe from 2016 and I just wonder about the effect of all that sugar. Not only on the system but on the teeth.
two questions there.
Thanks
The autonomic nervous system controls heat regulation, and people with CFS tend to have autonomic dysregulation such as orthostatic intolerance and heat intolerance.
Not really an answer as we don’t know exactly what causes the autonomic problems, except that that they can follow a virus, injury, surgery, pregnancy, concussion or vaccination. Bit they can also have a gradual onset with no identifiable cause.
Right but with ANS problems showing up in ME/CFS, long COVID, FM etc. finding out what’s causing it should be high on the list one would think. 🙂
I have wondered if I have POTs in addition to fibromyalgia and adrenal insufficiency. Have asked drs about testing for it and they say no need since I’m already taking fludrocortisone for the adrenal issue (take hydrocortisone), also take thyroid meds, and that fludrocortisone is the treatment for POTs. My BP is high and I take BP meds but my pulse is always high resting.. it goes to about 80s-90s when supine and in the 120s to 150s when upright. Another concern is if I lie down and then get up, my vision is super blurry… it takes ages to right the vision again to being less blurry.. could this be symptom of POTs? No eye dr can explain it nor can any other dr relate to the symptom. Thanks.
Yes, having altered vision when you move from lying down to sitting or standing can be a sign of orthostatic intolerance.
It’s true that fludrocortisone can help orthostatic symptoms, but there are several other medications and interventions that are often used in conjunction with fludrocortisone.
If your blood pressure and heart rate are normal during the NASA Lean Test or a tilt table test, but you still feel very sure you have orthostatic symptoms, you could have cerebral hypoperfusion.
This can be detected by having a transcranial Doppler ultrasound during a tilt table test. A few places have this additional monitoring. Have a look in the research or contact Dysautonomia International (which gave out grants for this equipment a couple of years ago).
You could also possibly have hypocapnia. This can also be tested for during a tilt table test by measuring end-tidal CO2.
For those too unwell to tolerate a standard tilt table test, van Campen, Visser and Rowe have proposed a less strenuous alternative protocol:
https://pubmed.ncbi.nlm.nih.gov/37252045/
https://www.healthrising.org/blog/2020/08/30/chronic-fatigue-syndrome-orthostatic-tolerance-dizziness/